Introduction:
- The term “vaccine” comes from the Latin Variolae vaccinae (cowpox), which Edward Jenner proved could prevent smallpox in humans in 1798. Today, the term “vaccine” refers to any biological preparation made from living organisms that boosts immunity against disease and either prevents (prophylactic vaccinations) or treats (in some situations) disease (therapeutic vaccines).
- A vaccine is an antigenic substance that stimulates adaptive immunity to a disease. Vaccines can protect against the effects of various infections.
- It contains a modified version of virus or bacteria that does not cause disease but “informs” our immune system what to do if the body is ever attacked by an actual, potentially harmful virus or bacteria.
- It is often regarded as the most effective means of preventing infectious infections. The material provided can be live but weakened types of bacteria or viruses, destroyed or inactivated versions of these pathogens, or purified material such as proteins.
- Vaccines are provided in liquid form via injectable, oral, or intranasal means.
Components of Vaccine:
The ingredients of a vaccination all play a crucial part in ensuring that the vaccine is safe and effective. Among these are:
Antigen
This is a dead or weakened form of a virus or bacteria that educates our bodies to recognize and fight the sickness if we come into contact with it again in the future.
Adjuvants
It helps to strengthen our immunological response. This suggests they help immunizations operate better.
Preservatives
It ensures that a vaccine remains effective. Stabilisers safeguard the vaccination during storage and shipment.
When vaccine ingredients are described on a labelling, they may appear unfamiliar. Many of the components used in vaccines, however, occur naturally in the body, the environment, and the foods we eat. All vaccine ingredients, as well as the vaccines themselves, are rigorously studied and monitored to assure their safety.

Fig: Composition of vaccine
Vaccination:
Vaccination is a method of delivering antigen to stimulate the immune response through active immunization. A vaccination is an immuno-biological material that is designed to provide specific protection against a certain disease. A vaccination is “antigenic,” but not “pathogenic.”
Principles of Vaccination
The fundamental purpose of vaccination is to develop protective immunity by creating a memory response to an infectious microbe using a non-toxic antigen preparation.
It is critical to generate the appropriate type of immunity, either antibody or cellular immunity.
Antibodies developed as a result of immunization are particularly effective against extracellular organisms and their products, such as toxins. Passively supplied antibodies have the same impact as produced antibodies.
Immunity:
The ability of the human body to tolerate the existence of material indigenous to the body (“self”) while eliminating outside (“non-self”) components. Because most bacteria are recognized as foreign by the immune system, this selective ability protects against infectious disease. The existence of antibody to a microorganism typically indicates immunity to that pathogen. Immunity is usually restricted to a single organism or a group of closely related organisms.

Fig: Body response to antigen
Immunity is acquired through two primary mechanisms:
Passive Immunity
Passive immunity refers to protection provided by an antibody or antitoxin produced by one animal or human and passed on to another. Passive immunity offers rapid protection against infection, but it is only temporary. The antibodies weaken over a few weeks to months, and the recipient is no longer protected.
The most prevalent type of passive immunity is that received by an infant from his or her mother. Antibodies, specifically IgG antibodies, are transferred through the placenta, primarily in the last 1 to 2 months of pregnancy. As a result, a full-term infant will have antibodies similar to the mother. Within the first few months following birth, these antibodies can protect the new born from some infections. Some infections (such as measles, rubella, and tetanus) are more protected by maternal antibodies than others (e.g., mpolio, pertussis).
Active Immunity
Active immunity is defence produced by a person’s own immune system. An antigen stimulates the immune system to create antibody-mediated and cell-mediated immunity. Active immunity, as opposed to passive immunity, typically lasts for many years, if not a lifetime. Surviving infection with the disease-causing form of the bacterium is one approach to gain active immunity. In general, once a person recovers from an infectious condition, they will have lifelong immunity to that disease (there are exceptions, e.g., malaria).
How do vaccines work?
The immune system attempts to create a response when a person is exposed to a disease-causing pathogen. Immunity is the result of a successful defence. An interaction with the bacteria or virus can cause sickness and its effects if the defence is unsuccessful. A specific germ is targeted by the body as it develops immunity, and as a result, antibodies are produced. This process passes with a “memory” of the experience that can be recalled for defence several months or years later. The antibodies that circulate in the bloodstream kill the germ the next time it is ingested, preventing it from causing sickness or minimizing the severity of the condition.
Because of this, a youngster who has had the measles is unlikely to contract it again. There is memory in the immune system. The antibodies produced during the first infection are prepared to neutralize and eliminate the virus the next time it is encountered by the child, prohibiting it from having a chance to infect them once again.
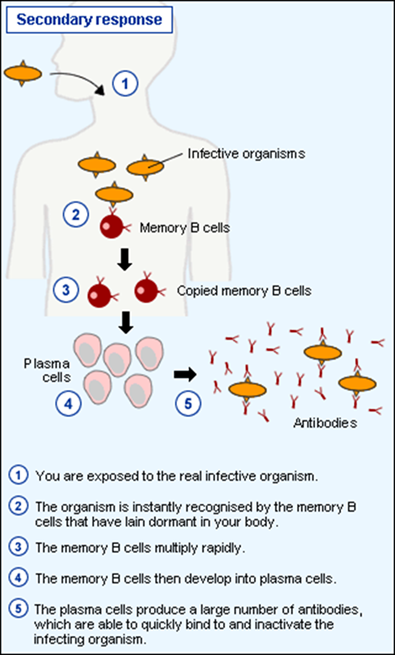
Fig: Working mechanism of vaccine
Types of vaccines:
Live vaccines
Live vaccines are made entirely from live infectious organisms. The only live vaccination is the “Variola” small pox vaccine, which is made of live vaccinia cow-pox virus, which is not pathogenic but antigenic, resulting in variola cross immunity.
Attenuated live vaccines
Pathogenic organisms that are virulent are treated to become attenuated and avirulent but antigenic. They no longer have the ability to cause full-blown illness, but they are still immunogenic.
Live attenuated vaccines should not be given to people who have a weakened immune system for the following reasons:
- Leukemia and lymphoma
- Other malignancies
- Receiving corticosteroids and anti-metabolic agents
- Radiation
- pregnancy
Inactivated (killed vaccines)
Heat or chemicals can kill or inactivate organisms, but they retain their antigenic properties. Although generally safe, they are not as effective as live attenuated vaccinations.

Fig: Different types of vaccines
Toxoids
They are made by detoxifying some bacteria’s exotoxins, turning them antigenic but not pathogenic. Adjuvants (such as alum precipitation) are used to boost vaccine potency.
Rather of acting on the organism, the antibodies created in the body as a result of toxoid administration neutralize the harmful moiety produced during infection. Toxoids, in general, are highly effective and safe immunizing drugs.
Polysaccharide and polypeptide (cellular fraction) vaccines
They are made from isolated cellular fractions, such as meningococcal vaccination from the polysaccharide antigen of the cell wall, pneumococcal vaccine from the polysaccharide found in the organism’s capsule, and hepatitis B polypeptide vaccine. Their efficacy and safety appear to be excellent.
Surface antigen (recombinant) vaccines
It is synthesized by cloning the HBsAg gene in yeast cells that express it. The HBsAg generated is then employed in vaccine formulations. Their efficacy and safety appear to be good as well.

Fig: Types of vaccines
Herd immunity
- It is also known as community immunity, population immunity, or mass immunity.
- This immunity arises when a large proportion of a community is immune to a disease (through vaccination and/or prior illness), making disease transmission from person to person uncommon. Because the disease has limited chance of spreading within the population, even those who have not been vaccinated (such as babies and the immunocompromised) benefit from some protection.
- Basically, it is the resistance of a group of individuals to an attack by a disease against which a large proportion of the group is immune.
- Individuals who are immune to a disease operate as a barrier in the spread of sickness, reducing or blocking disease transmission to others. Immunity can be developed naturally or artificially, for as through vaccination. When a crucial proportion of the population becomes immune, known as the herd immunity threshold (HIT) or herd immunity level (HIL), the illness may no longer survive in the population and cease to be endemic.
References:
- Hall, E., Wodi, A.P., Hamborsky, J., Morelli, V. and Schillie, S., 2021. Epidemiology and prevention of vaccine-preventable diseases. Centers for Disease Control and Prevention. Public Health Foundation. Retrieved January, 4, p.2022.
- Plotkin S. Vaccines, vaccination, and vaccinology. J Infect Dis 2003; 187:1347–59.
- Canouï E, Launay O. Histoire et principes de la vaccination [History and principles of vaccination]. Rev Mal Respir. 2019 Jan;36(1):74-81. French. doi: 10.1016/j.rmr.2018.02.015. Epub 2018 Dec 20. PMID: 30579659.
- Iwasaki, A. and Omer, S.B., 2020. Why and how vaccines work. Cell, 183(2), pp.290-295.
- The National Network for Immunization Information (www.immunizationinfo.org).
- Balakrishnan, S. and Rekha, V.B., 2018. Herd immunity: an epidemiological concept to eradicate infectious diseases. world, 6(9).
