Introduction to Cryptosporidiosis:
Cryptosporidia are coccidian parasites that have tropism for the microvillous region of the digestive epithelium and epithelium of respiratory organs of vertebrates. In immunocompetent individuals, Cryptosporidium parvum resolves on its own after causing a short-term diarrhea. However, in the immunocompromised patients, cryptosporidiosis can be life threatening.
The host is infected by the sporulated oocysts that are transferred with feces. Even after 2 weeks of resolving of diarrhea, the oocyts can still be shed in the feces of the previously infected person.
The thick walls of oocyst help them to resist the environment from destruction. It can be transmitted from person-to-person, by water-borne, animal-to-human and foodborne means. It can even survive in chlorine for many days.
Pathogenesis of Cryptosporidium parvum:
The exact methods by which C. parvum causes diarrhea are unclear. However, researches show s that C parvum alters intestinal epithelial cell function as well as the enteric immune and nervous systems.
The sporozoites of C. parvum adhere to intestinal epithelium and/or biliary cells to start an infection. For this, Gal/GalNAc epitopes must be present on intestinal epithelial cell glycoproteins and on the sporozoite surface.
After attachment, actin remodeling occurs initiating host kinase signaling pathways, enabling host invasion.
High levels of oocyst shedding in feces are typically linked to more serious damage to the intestinal lining. This includes villous atrophy and fusion, crypt hyperplasia, and infiltration of the submucosa by mononuclear and polymorphonuclear cells. Such damage is believed to impair the absorption of nutrients like carbohydrates, proteins, and vitamins (such as B12). Additionally, there is a decrease in the activity of brush border enzymes, such as lactase and sucrase, which is considered to have clinical significance.
Study of C parvum infection in intestinal tissue monolayer of mice and piglets and human have shown alteration of intestinal ion transport and/or increase gut permeability.
Pro-inflammatory cytokines (including TNF-a and IL-8) are predicted to promote leukocyte recruitment through the mucosa, resulting in the synthesis of inflammatory mediators such prostaglandins. It is well known that these inflammatory mediators, which are produced in reaction to a C parvum infection, promote intestinal secretion.
Cell damage and apoptosis have been noted in both in vitro studies and human intestinal tissues following C parvum infection, potentially playing a role in the development of the disease. Additionally, C parvum is thought to produce an enterotoxin that can trigger intestinal fluid secretion.
Clinical Features of Cryptosporidiosis:
The most common clinical feature of cryptosporidiosis in immunocompetent and immunocompromised persons is diarrhea, the symptom that most often leads to diagnosis.
Characteristically, the diarrhea is profuse and watery; it may contain mucus, but rarely blood and leukocytes, and it is often associated with weight loss. Other less common clinical features include abdominal pain, nausea and vomiting, and low-grade fever (<39°C). Occasionally, nonspecific symptoms such as myalgia, weakness, malaise, headache, and anorexia occur.
Both the duration of symptoms and the outcome typically vary according to the immune status of the host. AIDS patients usually experience a prolonged, life-threatening illness, whereas most immunocompetent persons experience a short-term illness with complete, spontaneous recovery.
Intestinal cryptosporidiosis
Typically, the duration of diarrheal illness and ultimate outcome of intestinal cryptosporidiosis depend on the immune status of the patient. In the most severely immunocompromised host, such as persons with AIDS, diarrheal illness due to Cryptosporidium infection of the gastrointestinal tract becomes progressively worse with time and may be a major factor leading to death. Fluid loss in patients with AIDS and cryptosporidiosis is often excessive; 3 to 6 liters of diarrheic stool per day is common, and as much as 17 liters of watery stool per day has been reported.
Respiratory cryptosporidiosis
Oocysts have been identified in sputum samples, tracheal aspirates, bronchoalveolar lavage fluid, brush biopsy specimens, and alveolar exudate obtained from lung biopsy. The symptoms associated with these infections include cough, shortness of breath, wheezing, croup, and hoarseness.
Gallbladder and biliary tree cryptosporidiosis
Gallbladder disease, primarily acalculous cholecystitis and, less frequently, sclerosing cholangitis, has been reported in HIV-infected patients. Symptoms include fever, right upper quadrant pain, nausea, vomiting, and simultaneous diarrhea. Jaundice may also occur with elevation in alkaline phosphatase and bilirubin.
Diagnosis:
Diagnosis based on clinical presentation is not reliable. Feces, water, food and tissue samples are tested for presence of oocysts of C parvum.
Concentration Method
A concentration technique using sucrose flotation with Sheather’s sugar solution (specific gravity: 1.26) can be employed. Cryptosporidium oocysts can then be examined under ×100 magnification to assess their internal structure.
Microscopic Examination
Ziehl–Neelsen (ZN) Staining
Both hot and cold ZN staining techniques can be used on fecal smears. In the hot method, the slide is covered with carbol fuchsin and gently heated until steam is visible. In the cold method, heating is skipped. After staining, the slide is rinsed under running water for 1–2 minutes, decolorized with 5% sulfuric acid for 30 seconds, and then counterstained with 3% methylene blue for one minute.
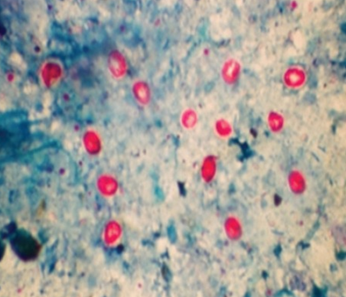
Figure: Round, pink Cryptosporidium parvum oocysts observed under Ziehl–Neelsen staining
Kinyoun’s staining method
The fecal smear is fixed with absolute methanol for one minute before staining. Kinyoun’s carbol fuchsin is applied for five minutes. The slide is then briefly rinsed with 50% ethanol (3–5 seconds), followed by distilled water. Decolorization is carried out using 1% sulfuric acid for two minutes, and the smear is counterstained with 1% methylene blue for one minute.
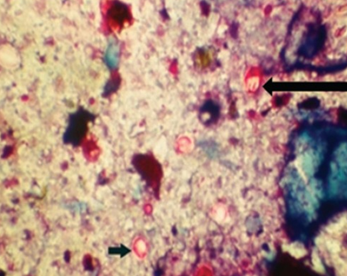
Figure: Round, red oocysts of Cryptosporidium parvum seen in Kinyoun’s acid-fast staining
Trichrome stain
Though this method may reveal the presence of oocysts, it is not suitable for definitive diagnosis, as the oocysts remain unstained. They appear as small, round bodies measuring approximately 4–6 μm in diameter.
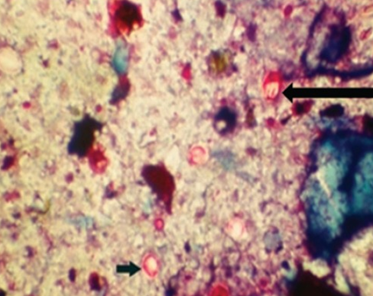
Figure: Cryptosporidium parvum oocysts ranging from 4 to 6 μm in size.
Immunological assays
For the identification of Cryptosporidium oocysts, immunological techniques are superior to light microscopy in a number of ways, including sensitivity and specificity.
Direct fluorescent antibody (DFA) assay
Many labs view this method as the gold standard since it provides the best sensitivity and specificity combination. It does not, however, offer an archiveable stained slide. Commercial test kits and a fluorescence microscope are needed.
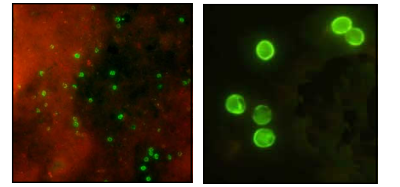
Figure: Cryptosporidium parvum oocysts under DFA
ELISA
In order to qualitatively identify Cryptosporidium-specific antigens in preserved stool specimens, enzyme immunoassays (EIAs) employ antibodies. It is more sensitive than conventional staining techniques and are easier to perform as well as more economical with shorter detection times.
Rapid antigen detection tests
More accurate, straightforward, and economical rapid antigen detection tests provide a viable substitute for routine testing. Although these assays are better than microscopic inspection, they necessitate several reagent additions, washing procedures, and incubations.
Two organisms can be distinguished in a single, fast test using the non-enzymatic rapid immunoassay Immuno Card STAT.
Method of nucleic acid detection
There may be benefits to using nucleic acid-based pathogen detection over traditional techniques.
Among their benefits are:
i) Determining which strains or species of recovered oocysts are host-specific. Whether the transmission is anthroponotic or zoonotic, the additional possible dangers are mostly determined by the mode of transmission.
ii) The identification of the specific source and severity of infections in epidemiological surveillance studies, and most importantly, the species genotyping for employing preventive measures, predominantly in the case of any outbreak.
Fluorescence in situ hybridization (FISH)
FISH (Fluorescence In Situ Hybridization) works by using fluorescent-tagged probes or short oligonucleotides that bind precisely to complementary sequences within the DNA or RNA of the organism being studied, allowing for direct visualization of specific genetic regions.
rRNA provides a potential target for nucleic acid probes, as elevated levels of rRNA is found in viable cells of the targeted organism.
FISH has the advantages of detecting and identifying pathogenic Cryptosporidium species in clinical, water and environmental samples within a 3-h time frame.
PCR techniques
Digital polymerase chain reaction
In digital PCR, the DNA sample is highly diluted and divided into numerous tiny compartments, ensuring that each compartment holds either a single copy or no copy of the target sequence before amplification begins. After PCR, the precise quantity of target DNA is calculated by comparing the number of compartments that show amplification (positive) to those that do not (negative). Loop mediated isothermal amplification (LAMP)
The method is driven by Bst DNA polymerase and a set of four carefully designed primers that recognize a total of six distinct sequences on the target DNA was used. Target of LAMP are SAM-1, hsp, gp60 genes of Cryptosporidium.
References:
- Centers for Disease Control and Prevention. Laboratory diagnosis of Cryptosporidiosis.
- https://www.cdc.gov/dpdx/resources/pdf/benchAids/Crypto_benchaid.pdf
- Rekha, K. M., Puttalakshmamma, G. C., & D’Souza, P. E. (2016). Comparison of different diagnostic techniques for the detection of cryptosporidiosis in bovines. Veterinary world, 9(2), 211–215. https://doi.org/10.14202/vetworld.2016.211-215
