Introduction:
Cancer is a term used to describe a wide range of illnesses that are all defined by the growth of abnormal cells that have the capacity to invade and kill healthy bodily tissue while also dividing uncontrolled.
Many tumors and the aberrant cells that make up the cancer tissue are further characterized by the name of the tissue from which the abnormal cells originated (for example, breast cancer, lung cancer, colorectal cancer).
Cancer does not only affect people; it may also affect animals and other living things.
Types of cancer:
Cancer is divided into two primary groups:
Leukemia, lymphoma, and multiple myeloma are hematologic (blood) cancers, which are malignancies of the blood cells.
Any other organ or tissue in the body can develop cancer, including solid tumors. Colorectal, breast, prostate, and lung cancers are the most prevalent types of solid tumors.
These tumors have similar characteristics, but their growth, spread, and treatment responses may differ. Certain tumors advance quickly. Some people’s growth is slower. Some have a higher likelihood of spreading to other bodily regions. Some people tend to continue where they left off. Surgery is the best course of action for some cancer kinds, whereas chemotherapy is more effective for other cancer types.
The three most prevalent malignancies in men, women, and children are as follows:
Men: Prostate, lung, and colorectal
Women: Breast, lung, and colorectal
Children: Leukemia, brain tumors, and lymphoma
Numerous variables, including age, gender, ethnicity, local environmental conditions, food, and genetics, have an impact on the frequency of cancer and the different forms of cancer.
As a result, these diverse variables affect both the incidence of cancer and the forms of cancer. For instance, the World Health Organization (WHO) provides the following general data regarding cancer worldwide:
The main cause of mortality globally is cancer. According to the most recent data from the WHO, it was responsible for 8.2 million fatalities, or around 22% of all deaths that were not caused by infectious illnesses.
The most cancer-related fatalities each year are caused by breast, colon, liver, stomach, and lung cancer.
Deaths from cancer worldwide are projected to continue rising, with an estimated 13.1 million deaths in 2030 (about a 70% increase).
Hallmarks of cancer:
Cancer cells have defects in both the feedback systems that regulate the control mechanisms and the regulation mechanisms that determine how frequently they divide (i.e. defects in homeostasis).
Although normal cells divide and develop, there are several controls on that proliferation. They can only multiply when growth factors are available. A molecular brake prohibits them from dividing if they are damaged until they are fixed. They commit programmed cell death if they cannot be corrected (apoptosis).
A methodology for simplifying the enormous complexity of cancer phenotypes and genotypes into a preliminary group of fundamental principles is the hallmarks of cancer concept.
- Sustaining proliferative signaling
- Evading growth suppressors
- Resisting cell death
- Enabling replicative immortality
- Inducing angiogenesis
- Activating invasion and metastasis
- Deregulating cellular energetics and metabolism
- Avoiding immune destruction

Fig: Hallmarks of cancer
Carcinogen:
A chemical, organism, or agent capable of causing cancer is referred to as a carcinogen. UV radiation from sunlight and some viruses are examples of environmental carcinogens that occur naturally. Humans can also produce carcinogens (such as automobile exhaust fumes and cigarette smoke).
Any material, radionuclide, or radiation that promotes the formation of cancer is known as a carcinogen. This could be as a result of its capacity to alter the genome or to interfere with cellular metabolic processes. The majority of carcinogens cause mutations in cells by interacting with their DNA.
There are several naturally occurring carcinogens. Aflatoxin B1, a strong, naturally occurring microbial carcinogen generated by the fungus Aspergillus flavus growing on stored grains, nuts, and peanut butter, is an example of a potent, naturally occurring microbial carcinogen.
Human cancer has been linked to viruses such as hepatitis B and the human papillomavirus. Rous sarcoma virus, discovered by Peyton Rous in 1910, was the first to be proved to cause cancer in animals. Some bacteria, such as Helicobacter pylori, and helminths, such as Opisthorchis viverrini and Clonorchis sinensis, are also known to cause cancer in humans.
Chemical Carcinogens
These include substances such as tobacco smoke, asbestos, benzene, formaldehyde, arsenic, vinyl chloride, and certain pesticides.
Physical Carcinogens
Ionizing radiation, such as X-rays and gamma rays, and ultraviolet (UV) radiation from the sun or tanning beds are examples of physical carcinogens.
Biological Carcinogens
Certain viruses and bacteria are known to contribute to the development of cancer. For example, human papillomavirus (HPV) can cause cervical cancer, and hepatitis B and C viruses can lead to liver cancer.
Occupational Carcinogens
Substances found in certain workplaces can be carcinogenic. Examples include asbestos, benzene, cadmium, chromium, and diesel engine exhaust.
Lifestyle-related Carcinogens
Factors such as tobacco smoke, unhealthy diet, excessive alcohol consumption, obesity, and lack of physical activity can increase the risk of developing cancer.

Fig: This figure describes the process of carcinogenesis as a result of viral integration into the cell genome.
Co-carcinogens are substances that, although not causing cancer on their own, do increase the action of other carcinogens in creating cancer.
Carcinogens, sometimes referred to as cancer-causing substances, exist in three different types:
- Procarcinogens are substances that induce cancer owing to changes in metabolism.
- Cytochrome P450-dependent monooxygenases metabolize the majority of recognized carcinogens. Because these enzymes are required for the activation of procarcinogens, variations in the genes that encode these enzymes influence individual susceptibility to carcinogenesis.
- Cocarcinogens are chemicals that cause cancer by interacting with another substance.
When cocarcinogens are combined with a carcinogen, they increase tumorigenicity. Tumor promoters and cocarcinogens, in general, do not have tumorigenic action.
- Direct acting carcinogens, which can cause cancer in and of themselves. Alkyl or aryl epoxides, nitrosoureas, nitrosamides, and some sulfonate and sulfate esters are examples of direct-acting carcinogens.

Fig: This figure describes the process of carcinogenesis as a result of chemical exposures (ie. smoking)
Stages of cancer:
Basically, cancers have several four stages. The size and location of the tumor are two of the criteria that affect the specific stage.
Stage 0
There are primarily abnormal cells at this stage that have the potential to develop into cancer, not actual cancer. No neighboring tissues have been affected by them. Most cancers at this stage are treatable and most tumors can be completely removed surgically.
Stage I
In this stage cancer is localized to a small area and hasn’t spread to lymph nodes or other tissues.
Stage II
Although the cancer has grown, it has not yet spread.
Stage III
The cancer has grown severe and it may have migrated to the lymph nodes or other tissues.
Stage IV
Other bodily parts or organs have become infected with cancer. Advanced cancer or metastatic cancer are other names for this stage.

Fig: Cancer Progression and Metastasis
Cancer cells that separate from the primary tumor and travel through the circulation or lymphatic system to other parts of the body are referred to as metastatic cancer.
Metastatic tumors (metastases) can occur in three ways:
- They can grow directly into the tissue surrounding the tumor.
- Cancer cells can travel through your bloodstream to distant locations in your body.
- Cancer cells can travel through your lymph system to nearby or distant lymph nodes.

Fig: Breast cancer to breast metastasis
The development of metastases distant from the primary tumor requires the performance of a long series of events. Breast cancer cells must first detach themselves from the primary tumor, then enter the circulation (intravasation), and travel through the body by following the blood vessels. They then have to get out of these vessels (extravasation) and colonize a new organ (brain) where they multiply and eventually develop into secondary tumors (metastases).
Cancer genes:
Tumor cells differ from their normal progenitors due to genetic changes that influence growth-regulatory genes, which makes cancer a hereditary illness.
These cancer genes may be divided into two categories: oncogenes, which act as positive growth regulators, and tumor suppressor genes, which act as negative growth regulators.
Tumor suppressor genes
Tumor suppressor genes represent the contrasting component of cell growth regulation, often operating to prevent tumor formation and cell proliferation. These genes are frequently deleted or inactivated in tumors, which removes the anti-proliferative controls and aids in the irregular growth of tumor cells.

Fig: Tumor Suppressor Genes and Proto-oncogenes
Oncogenes
A mutant gene that is capable of causing cancer is known as an oncogene.
Proto-oncogenes play a part in controlling regular cell division and are the form of oncogenes before they are altered to oncogenes. A mutation in proto-oncogenes into an oncogenes result in cancer by producing an uncontrollable increase in cell division and growth.

Fig: Methods of Oncogene Activation in Cancer
Cell Death Mechanisms in Cancer:
Apoptosis: Apoptosis is a type of programmed cell death that occurs when cells are no longer needed or are damaged beyond repair. It is characterized by the fragmentation of the cell’s DNA, the condensation of the cytoplasm, and the formation of apoptotic bodies that are phagocytosed by nearby cells. Apoptosis is controlled by a series of proteins known as caspases, which are activated in a cascade by various stimuli, such as DNA damage or immune cell signaling.
Necrosis: Necrosis is a type of cell death that occurs when cells are damaged by physical injury, chemical toxicity, or infection. It is characterized by the swelling and rupture of the cell membrane, the release of intracellular contents into the extracellular space, and the activation of the immune system. Necrosis is not a regulated process and can be harmful to surrounding tissues.
Autophagy: Autophagy is a process by which cells degrade and recycle their own damaged or unnecessary components. It is controlled by a series of proteins known as autophagy-related proteins (ATGs). Autophagy can serve as a protective mechanism against stress and can help to maintain cellular homeostasis. However, excessive autophagy can lead to cell death.

Fig: Cell Death Mechanisms in Cancer
Anoikis: Anoikis is a type of apoptosis that occurs when cells are detached from the extracellular matrix (ECM), their normal microenvironment. Cancer cells often evade anoikis by expressing proteins that promote their attachment to the ECM or by activating signaling pathways that promote their survival.
Senescence: Senescence is a state of permanent cell cycle arrest that occurs when cells are damaged or reach their replicative capacity. It is characterized by the activation of p53 and p16INK4a, the expression of senescence-associated secretory phenotype (SASP) factors, and the presence of senescence-associated heterochromatic foci (SAHF). Senescent cells do not divide but can still secrete various factors that can influence the microenvironment and contribute to cancer development.
Warning Signs of Cancer:
- Alterations affecting the size, shape, consistency, or color of stools. (constipation, diarrhea)
- Unusual bleeding or discharge
- Blood in the stools or pee
- Discharge from your nipples, penis, or other bodily regions.
- wound that never gets better
- Breast or other body part lump
- Persistent coughing and bloody sputum from the throat
- Discomfort during swallowing due to a pressing sensation in the chest or throat
Detection method of Cancer:
- Sequencing
- Amplification Technique
- Microarray
- Tissue microarray analysis
- Protein array
- Tissue microarray Visualization
Prevention:
Implementing current evidence-based preventative techniques and reducing or avoiding significant risk factors might save between 30% and 50% of cancer deaths. Early cancer identification and treatment of cancer patients can both minimize the burden of the disease. Additionally, prevention is the most efficient long-term approach to the control of cancer.
- Modifying or avoiding the following key risk factors can help prevent cancer:
- Do not use tobacco products, such as cigarettes or smokeless tobacco.
- keep a healthy weight and consume a balanced diet rich in fruits and vegetables.
- Regular exercise, limiting alcohol intake, and practicing safe sex
- Immunized against the human papillomavirus and hepatitis B (HPV)
- Reducing UV exposure preventing unwanted ionizing radiation exposure (e.g. minimize occupational exposure, ensure safe and appropriate medical use of radiation in diagnosis and treatment)
- Regular medical attention
- Some persistent infections might increase your chance of developing cancer. Chronic infections increase the risk of cancer development in people living in low- and middle-income nations.
Management:
Cancer is more likely to respond to effective treatment when identified early, resulting in a greater probability of surviving as well as less morbidity and less expensive treatment.
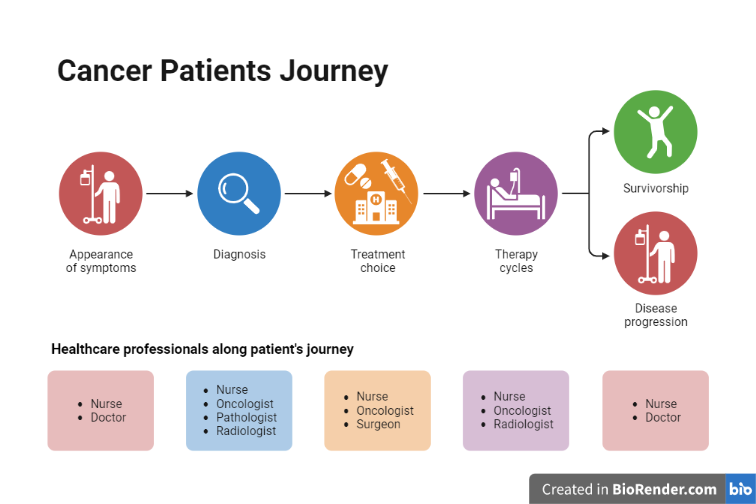
Fig: Cancer Patients Journey
There are two distinct strategies that promote early detection:
Early diagnosis identifies symptomatic cancer cases at the earliest possible stage.
Screening aims to identify individuals with abnormalities suggestive of a specific cancer or pre-cancer who have not developed any symptoms and refer them promptly for diagnosis and treatment.
Treatment options include surgery, cancer medicines and/or radiotherapy, administered alone or in combination. A multidisciplinary team of cancer professionals recommends the best possible treatment plan based on tumor type, cancer stage, clinical and other factors. The choice of treatment should be informed by patients’ preferences and consider the capacity of the health system.
Palliative care, which focuses on improving the quality of life of patients and their families, is an essential component of cancer care. Survivorship care includes a detailed plan for monitoring cancer recurrence and detection of new cancers, assessing and managing long-term effects associated with cancer and/or its treatment, and services to ensure that cancer survivor needs are met.
Major Treatment Modalities:
There are several major treatment modalities for cancer, which may be used alone or in combination, depending on the type and stage of the cancer and the overall health of the patient.
Surgery: Surgery involves the removal of the cancerous tissue or organ. This can be done through various techniques, such as open surgery, laparoscopic surgery, or robotic surgery.
Radiation therapy: Radiation therapy uses high-energy beams, such as X-rays or protons, to kill cancer cells or shrink tumors. It can be delivered externally or internally, depending on the location of the cancer.
Chemotherapy: Chemotherapy involves the use of drugs to kill cancer cells or stop them from dividing. It can be administered orally or intravenously, and may be given as a single agent or in combination with other drugs.

Fig: Basic methods of chemotherapy
Immunotherapy: Immunotherapy involves the use of drugs or other substances to boost the body’s immune system to attack cancer cells. This can include monoclonal antibodies, checkpoint inhibitors, and other agents.
Targeted therapy: Targeted therapy involves the use of drugs that specifically target the abnormalities or mutations present in cancer cells. This can be more effective and have fewer side effects than chemotherapy.
Hormone therapy: Hormone therapy involves the use of drugs or other agents to block the production or action of hormones that can fuel the growth of certain types of cancer, such as breast and prostate cancer.
Stem cell transplant: A stem cell transplant involves replacing damaged or destroyed bone marrow with healthy stem cells to help restore the body’s ability to produce blood cells. It is often used in the treatment of certain types of cancer, such as leukemia and lymphoma.

Fig: Most common methods of cancer therapy
References:
- Eggert J. (Ed). Cancer Basics. (2nd ed.). Pittsburgh, PA: Oncology Nursing Society; 2017. National Cancer Institute. Cancer staging. Cancer.gov. https://www.cancer.gov/aboutcancer/understanding/what-is-cancer. Updated March 9, 2015. Accessed November 6, 2020.
- Vogt PK. Cancer genes. West J Med. 1993 Mar;158(3):273-8. PMID: 8460509; PMCID: PMC1311753.
- National Cancer Institute. What is cancer? Cancer.gov. https://www.cancer.gov/aboutcancer/understanding/what-is-cancer. Updated February 9, 2015. Accessed November 6, 2020.
