Introduction:
Microorganisms are ubiquitous. Microbes grow and multiply under favorable conditions. In laboratory, for the purposes of study, they are allowed to grow and multiply. So, it always becomes necessary to remove or destroy microbes from materials or from areas because they are responsible for causing contamination, decay, and infection. This is the main object of sterilization. Control of microorganisms is essential in many situations:
- To prevent the transmission of pathogenic microorganism and to check the disease spread.
- To prevent the contamination of pure cultures in scientific and microbiology laboratories.
- To prevent spoilage and decomposition and food and food products.
- To ensure safety from contaminating organisms in pharmaceutical industries.
- To prevent the microbial contamination in industrial process.
- To maintain aseptic condition for surgery.
Sterilization is defined as the process by which an article, surface or medium is freed of all microorganism either in vegetative state or in spore state.
The method of sterilization used would depend on the purposes for which sterilization is carried out, the material which has to be sterilized and the nature of microorganism that are to be removed or destroyed. The various agents used in sterilization are categorized into two main groups-physical agent and chemical agents.
Physical method of sterilization:
Sunlight
Sunlight possesses appreciable bactericidal activity and plays an important role in the spontaneous sterilization under natural conditions. This action is mainly due to its content of ultraviolet rays, under natural conditions, its sterilizing power varies according to the situations and circumstances.
Drying
Drying has a deleterious effect on microorganisms as moisture is very essential for the growth of bacteria. However, the power of sterilization power varies with different bacteria and also with conditions under which they are exposed to drying. Spores are unaffected by drying.
Heat
The most reliable method of sterilization is heat. Heat sterilization is the method of choice, only the materials damageable by heat are not sterilized by this method, or sterilized at lower temperature for longer periods or by repeated cycles.
Many factors influence the sterilization by heat. They are as follows:
- Nature of heat- dry heat or moist heat
- Temperatures and time of sterilization
- The number of microorganism present
- Nature of microorganism, i.e., vegetative cells or spore cells.
- The characteristics of microorganism like species, strain, sporing capacity.
- The type of material from which the microorganisms have to be eradicated.
Dry Heat
The killing effect of dry heat is due to protein denaturation, oxidative damage and the toxic effect of elevated levels of electrolytes. In microorganisms are more resistant to heat. They are killed when oxidation of the cell constituents occurs, which requires very high temperatures. Depending upon the material to be sterilized, various methods of dry heat sterilization are available.
Flaming
For sterilizing inoculating loops, points of forceps searing spatulas and are heled in Bunsen flame till they become red hot. It is always recommended to dip the loop containing infective proteinaceous materials in chemical disinfectants, before flaming to prevent spattering. Moreover, in order to destroy bacteria from the mouths of culture tubes, glass slides, cover slips, etc. it is always recommended to pass it a several times through the flame of Bunsen without allowing them to become red hot. However, this methos is unsatisfactory.
Hot air oven
Hot air oven is the most widely method of sterilization by dry heat. It is used to sterilize glassware, forceps, scissors, scalpels, all glass syringes, swabs paraffin, sulphonamides, dusting powder, fat, greases, etc. Glass wares should be perfectly with cottonwool and other glassware like Petri dishes and pipettes should be wrapped in craft before being placed in the hot air oven.
It consists of an insulated double walled cabinet heated by electricity and it is constructed to withstand high temperature. There is a fan fitted either at the bottom or back to circulate hot air inside the chamber. A thermostat regulates the temperatures at the desired level and a thermometer is fitted for recording the temperature.
Moist heat
Sterilization by dry heat is not as efficient as by moist heat. The mechanism by which organism are killed by moist heat is different form that of dry heat. Denaturation and coagulation of protein is the major causes of the effect by moist heat. When the steam condenses on the cooler surfaces, it liberates at latent heat, which raises the temperatures of that surface. In the case of the spore, steam condenses on it, increases its water content with ultimate hydrolysis and breakdown of the bacterial protein. There are various methods of moist heat sterilization. They are:
- Temperatures below 100oc
- Temperatures at 100oc (Boiling)
- Steam at atmospheric pressure (100oc)
- Steam under pressure
Filtration
Filtration is a physical method of removing microorganism from solutions or gases. The ability of porcelain filters to remove bacteria from solutions was known in 19th century. The effectiveness of a filter will depend on the pore size. Recently, porcelain filters have been replaced by membrane filters that is composed of cellulose acetate, polycarbonates and other polymers. These filters are very thin and are available with known pore sizes. They are relatively inert and absorb very little fluid. These filters are used to sterilize liquids which cannot be heat sterilized such as beer, wine other alcoholic beverages, serum, and other solutions used in the preparation of culture media.
Ultrasonic and sonic vibration
Both the ultrasonic and sonic vibrations possess the bactericidal activity, however, their results are variable. Microorganisms vary in their sensitivity to them and hence this method is of no practical value in sterilization technique.
Radiation
The effectiveness of the radiation depends on the presence of enzymes within the organisms which can repair the damage, degree of susceptibility of microorganisms, presence of oxygen, water, and other chemicals.
They are two types of ionizing and non-ionizing radiation.
- Ionizing radiation such as cosmic rays, X-rays, gamma rays, are highly lethal to DNA and other vital cell constituents and causes biological damage by producing hyper reactive ions. They have very high penetration power. Since, there is no appreciable increases in temperature, this method is referred as cold sterilization. Gamma radiation is used for sterilization of plastics, syringes, swabs, culture plates, cathedral, animal feeds, oil, greases, fabrics, and metal foils.
- Nonionizing radiations such as infrared and ultraviolet rays are used for disinfecting enclosed areas such as entryways, hospital wards, operation rooms, inoculation rooms and laboratories.
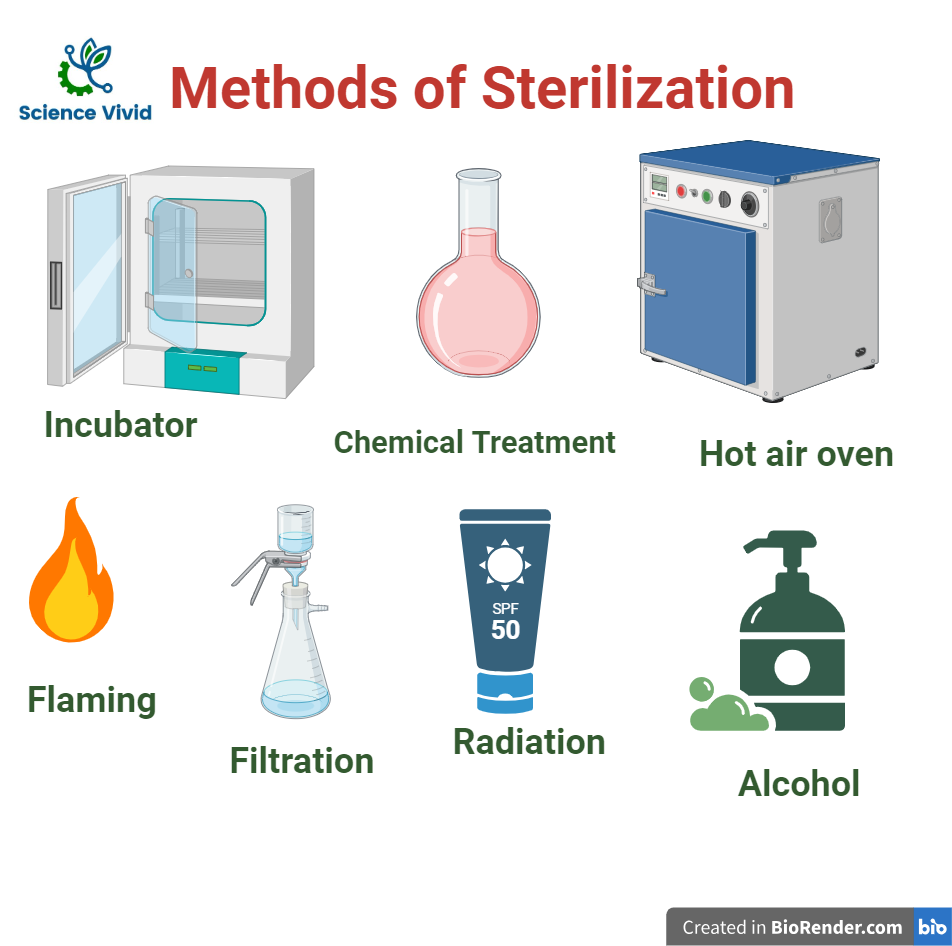
Fig: Methods of Sterilizaton
Chemical Methods:
Different chemicals are employed for the purpose of sterilization. A variety of factor determine the potency of chemical agents such as its concentration, time of action, mode of action pH of the medium, temperature, nature of the organisms and presence of extraneous materials. These chemical agents act in various ways such as protein coagulation, disruption of the cell membrane, removal of functional groups which are essentials for proper functioning of the enzymes and substrate concentration.
These chemical agents include halogens, phenolics, alcohols, heavy metals.
Halogens
Among the halogens, iodine and chlorine are the most important and are used in chemical sterilization because both are strong oxidizing agents. Generally, chlorine is used in water purification in water supplies, swimming baths, food and diary industries, etc., Chlorine have a wide spectrum of activity against virus. Iodine is used as a local antiseptic. It is an active bactericidal agent with a moderate activity against spores.
Dyes
Aniline and acridine dyes are groups of dyes that are used extensively as skin and wound antiseptics. In higher dilution, both are bacteriostatic. Brilliant green, malachite green and crystal violet are the highly used aniline dyes.
Phenols
These are obtained by distillation of coal tar. It inactivates cells by disrupting the cell membrane irreversibly and cause cell lysis. In addition, phenol and its derivates are commonly used in surgical and hospital sanitation environments. However, care must be taken while using phenolics since these can damage the skin and tissues.
Heavy Metals
It causes cell inactivation. One of the first metal used was arsenic, but due to its toxic properties, it is not generally used now-a days. Moreover, other heavy metals used are silver nitrate, copper sulphate, mercuric chloride and potassium permanganate.
Aldehydes
Formaldehyde is one of the oldest disinfectants known. It inactivates microbial proteins by oxidation of the amino groups. In aqueous solutions, it is markedly bactericidal and sporicidal and also has a lethal effect on virus. It is used to preserve anatomical specimens and for destroying spores in hair and wool.
Alcohols
Most commonly used alcohols for disinfectant are ethyl alcohol and isopropyl alcohol. These are the mild disinfectants and are non-toxic when used for external application as antiseptics. They act by denaturing bacterial proteins.
Gases
Fumigation of Sulphur, formaldehyde, ethylene oxide are generally used for sterilization.
