Introduction to Shigella:
Shigella are the cause of bacillary dystentery exclusively facultative intracellular pathogens in intestine of humans and other primates. Shigella are slender (1-3 × 0.5 µm in size) Gram-negative rods belonging to the family Enterobacteriaceae. They are non-motile bacterium, non–sporulating and non-capsule formers. The genus Shigella comprises four different species; S. dysenteriae, S.flexneri, S. boydii and S. sonnei.
Growth Characteristics of Shigella:
Shigella spp are facultative anaerobes and can grow in various culture media.
Nutrient Agar
Colonies are Convex, circular, transparent colonies with intact edges reach a diameter of about 2 mm in 24 hours
Mc Conkey Agar (MAC)
Colonies appear as convex, Non-Lactose Fermenting (NLF) colorless colonies about 2 -3 mm in diameter (except for S. sonnei, flat colonies and late lactose fermenter)
Xylose Lysine Deoxycholate (XLD) Agar
Colonies appear as transparent pink or red smooth colonies 1 -2 mm in diameter. On both MAC and XLD, S. dysenteriae colonies are smaller than other Shigella spp. Salmonella Shigella (SS) agar is not use as it frequently inhibits the growth of S. dysenteriae serotype.
Hektoen Enteric (HE) Agar
HE agar is a differential selective agar that is useful for isolation of Shigella. Shigella form green colonies.
Biochemical Characteristics of Shigella:
They are Catalase test positive (except S. dysenteriae type 1). They are glucose fermenters with production of acid only (except S. flexeneri type 6, S. boydii 13 and 14 and S. dysenteriae 3 produce both acid and gas). They are non-lactose fermenter (except S. sonnei)
Virulence Factors of Shigella:
Type III Secretion System (T3SS)
The 30 kb Mxi-Spa, type III secretion system (TTSS), and invasion plasmid antigens (IpaA, IpaB, IpaC, and IpaD) are encoded by the plasmid to allow the bacteria to invade colonic and rectal epithelial cells and release themselves into the cytosol of the host cell. IpaB specifically causes host macrophages and dentritic cells to undergo apoptosis.
Intracellular Spread Protein (IcsA)
IcsA is a surface protein that facilitates actin-based motility, which is necessary for the bacterium to move both within and between cells.
Shiga Toxin
S. dysenteriae type 1 produces a potent exotoxin in trace amounts that inhibits protein synthesis by deactivating the 60s ribosome. This toxin, which comprises one A subunit and five B subunits, is the same as verotoxin-1, which is produced by enterohemorrhagic strains of E. coli. The harmful component of Shiga toxin is the A subunit. The A subunit is transferred into the cell more easily when the B subunits attach to a host cell glycolipid (Gb3). Damage to the intestinal epithelium is the main sign of toxin action. Because the toxin destroys the capillaries of the lamina propria of the intestinal villi, resulting in ischemia and hemorrhagic colitis, Shigella that produce Shiga toxin cause more severe illness.
Endotoxin
Upon autolysis, all Shigellae release their toxic lipopolysaccharide. This endotoxin probably contributes to the irritation of the intestinal wall.
Iron Chelation Systems
While S. dysenteriae and certain S. sonnei isolates express enterochelin, the majority of isolates of S. flexneri and S. sonnei exhibit aerobactin siderophores. They can extract ferric ions from their physiological carriers, lactoferrin and transferrin, because they have a strong affinity for them. Both types can be expressed by certain isolates.
Pathogenesis of Shigella Infection:
Transmission
Transmission of Shigella occurs through the fecal-oral route.
Incubation Period
Incubation ranges from 12 hours to 4 days.
One important factor influencing the illness is capacity of Shigella to penetrate and colonize the intestinal epithelium. Shigellosis is characterized by a brief episode of watery diarrhea accompanied by cramping in the intestines and overall malaise, which is quickly followed by the release of bloody, mucoid, frequently mucopurulent feces. The gastrointestinal tract is nearly always the only organ affected by Shigella infections. The majority of what is now known about mechanisms comes from research on S. flexneri. The invasive pathogen S. flexneri infection is a multi-step process. S. flexneri passes through the intestinal epithelium, which developed as a functional and physical barrier to keep commensal and pathogenic bacteria out of the body, in order to reach the intestinal mucosa.
Entry via microfold cells (M cells)
S. flexneri appears to trigger its absorption into microfold cells (M cells) and transcytose across the epithelial layer during the early stages of infection rather than invading the epithelial barrier from the apical side. M cells are specialized epithelial cells that continuously collect particles from the intestinal lumen and transport them to the mucosal lymphoid tissue underneath, where immune responses might be triggered. Early actin cytoskeleton reorganization is induced by binding, preparing the cell for uptake. Following transcytosis, S. flexneri is discharged into an intraepithelial pocket where it encounters resident macrophages that engulf and break down incoming material. This process is facilitated by the Mxi-Spa T3SS and translocator proteins IpaB, IpaC, and IpaD, which allow the bacteria to escape from the phagosome and enter the cytoplasm.
Escape from Phagosome
The S. flexneri quickly induces apoptosis in macrophages to ensure its survival (IpaB). After being freed from the dying macrophage, S. flexneri can enter epithelial cells from the basolateral side, get out of the phagosome, and multiply inside the cytoplasm.
Intracellular Survival and Spread
Shigella spp. produce significant tissue degradation that impairs the adsorption of water, nutrients, and solutes. This can lead to watery diarrhea and the blood and mucus in stools that are typical of shigellosis. Diarrheal illnesses are characterized by a disruption of electrolyte homeostasis and modifications in membrane transport mechanisms, such as unchecked ion and fluid secretion.
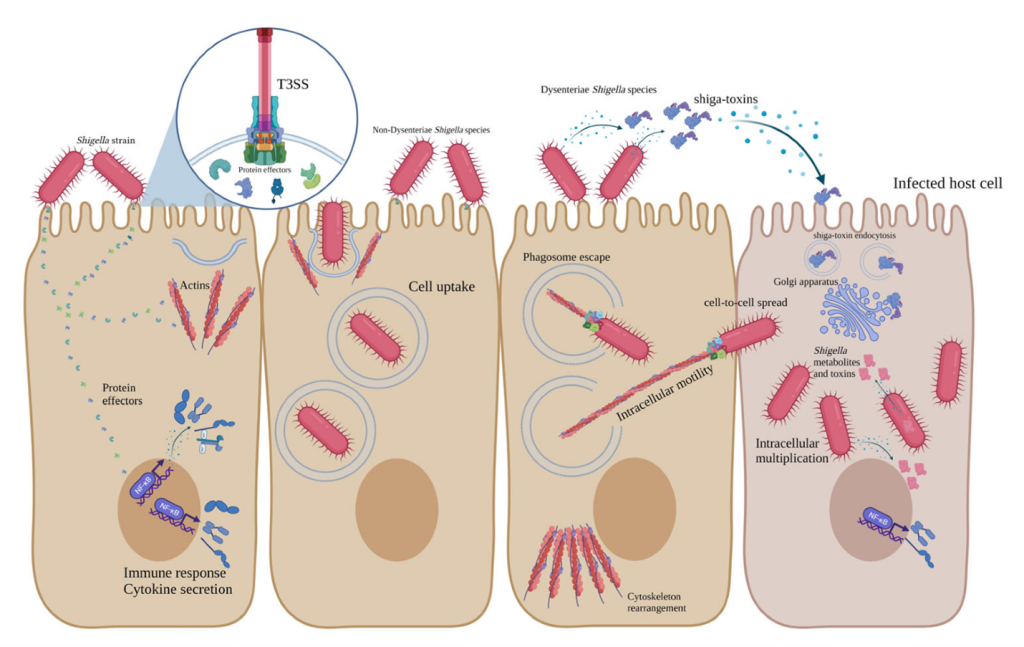
Fig: Pathogenesis of Shigella
