Introduction and epidemiology:
Ramsay Hunt syndrome (RHS) is a rare neurological disorder occur when a shingles outbreak affects the facial nerve (facial palsy) near one of your ears. In addition to this painful rash, it can cause facial paralysis and hearing loss in the affected ear. Tinnitus (ringing in the ears) and hearing loss are two examples of ear disorders that can also occur.
In 1907 the American neurologist and army officer in World War I (James Ramsay Hunt) described three different neurological syndromes and the most famous of which is the second, which is known as “Ramsay Hunt syndrome.
Ramsay Hunt syndrome type 2 is consequence of the infection of geniculate ganglion by varicella zoster virus (VZV), the same virus that causes chickenpox in children and shingles (herpes zoster) in adults. The previously latent (inactive) varicella-zoster virus gets revived in patients with Ramsay Hunt syndrome and spreads to harm the facial nerve.
The incidence of RHS is 5 /1,00, 000 people and most affected patients are within age group of (20-30) years with no gender prediction. Although it is rare, it is more commonly found with immunocompetent and immunocompromised patients. In addition, stress, chemotherapy, immunocompromise, infection, starvation, and other factors that enhance the risk of herpes zoster too will increase the possibility of Ramsay Hunt syndrome. Ramsay Hunt syndrome can be acquired by anyone who has had chickenpox. The majority of instances, however, affect seniors, particularly those over the age of 60. Children with the Ramsay Hunt syndrome are relatively uncommon.
Pathophysiology:
Early stages of VZV infection cause diffuse vesicular rash, with fever a condition that is commonly referred to as chickenpox. The virus is transmitted by respiratory droplets during the acute phase of the infection. After the initial infection, the virus will often remain dormant in the sensory ganglion of the spinal and cranial nerves. During times of physiological stress or immunocompromise subsequent reactivation of the virus causes a “zoster” or “herpes zoster” phenomenon.
Sign and Symptoms:
The facial nerve is frequently paralyzed (palsy), and an ear rash is common in those who are affected. These two signs don’t always appear at the same time. Only one side of the face is usually injured in the majority of cases (unilateral).
Exterior region of the ear (pinna) and often the external ear canal are afflicted by a reddish (erythematous), itchy, blistering (vesicular) rash in most cases of Ramsay Hunt syndrome.
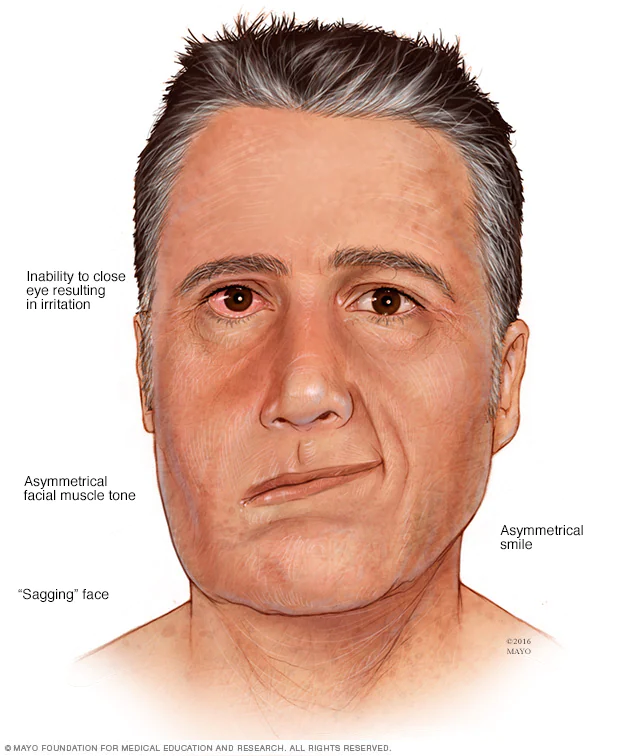
Facial droop and paralysis on one side of the face, as well as difficulties closing one eye, eating (food falls out of the weak corner of the mouth), difficulty in expression, and fine motions of the face are causes due to weakness on one side of the face.
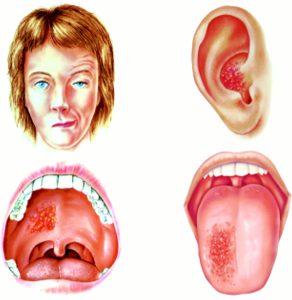
Fig: Clinical features of Ramsay Hunt syndrome. Note peripheral facial weakness characterised by a widened palpebral fissure and decreased forehead wrinkling and smile on the right, often associated with vesicles in the ipsilateral ear, on the hard palate, or on the anterior two thirds of the tongue.
Diagnosis:
Inflammation surrounding the geniculate ganglion of the damaged facial nerve should be detectable on magnetic resonance imaging (MRI). The extent of cranial nerve involvement can be determined by audiometry, vestibular testing, and flexible fiberoptic laryngoscopy. Imaging and serological investigations may be useful when the causes of initial facial paralysis are unknown clinically, however most cases of Ramsay Hunt syndrome are apparent.
The history, clinical symptoms, and neurological examination are all used to make a diagnosis of Ramsay Hunt syndrome. The fluid obtained from the vesicles can be examined microscopically using the Tzanck smear technique in the early stages. The test’s sensitivity is poor, but its specificity is high when symptoms occurrence is high prior to the test.
Since, herpes simplex, varicella-zoster, and CMV infections all are herpesviruses, it is very challenging to distinguished them through culture. VZV can also be cultured or characterized by polymerase chain reaction (PCR) testing using the sample collected from ear scrapings, tears, saliva, blood mononuclear cells, or cerebrospinal fluid.
Prevention:
Children are now routinely vaccinated against chickenpox, dramatically reducing the risk of infection. A shingles vaccine for people ages 50 or older also is recommended. Patients with active vesicles should also avoid contact with unvaccinated or immunocompromised individuals, as their lesions can spread the varicella-zoster virus. Lastly, administering the shingles vaccine likely prevents Ramsay Hunt syndrome as well, but the vaccine is not 100% effective.
Treatment:
The major goals of treatment are to reduce late complications such spastic facial paralysis and postherpetic neuralgia. Significant decrease in long-term complications with the use of strong anti-inflammatory drugs with a combination of acyclovir and prednisone is reported to be effective. Antiviral medications like acyclovir or valacyclovir may be administered.
If the pain persists despite the use of steroids, powerful medications may be advised. While there will be a weakness of the face it is suggested to wear an eye patch to prevent injury to the cornea and other damage to the eye if the eye does not close completely. To keep the eye from drying out, some people use a specific eye lubricant at night and artificial tears during the day. In the absence of randomized controlled trials, RHS is treated empirically with an oral combination of antiviral medications and steroids. RHS, on the other hand, has a worse prognosis than Bell’s palsy (idiopathic facial palsy).
References:
- Sweeney CJ, Gilden DH. Ramsay Hunt syndrome. J Neurol Neurosurg Psychiatry. 2001 Aug;71(2):149-54.
- Sommer T, Karsy M, Driscoll MJ, Jensen RL. Varicella-Zoster Virus Infection and Osteomyelitis of the Skull. World Neurosurg. 2018 Jul; 115:297-300.
- Jeon Y, Lee H. Ramsay Hunt syndrome. J Dent Anesth Pain Med. 2018;18(6):333-337. doi:10.17245/jdapm.2018.18.6.333
- Paiva ALC, Araujo JLV, Ferraz VR, Veiga JCE. Facial paralysis due to Ramsay Hunt syndrome – A rare condition. Rev Assoc Med Bras (1992). 2017 Apr;63(4):301-302.