Introduction:
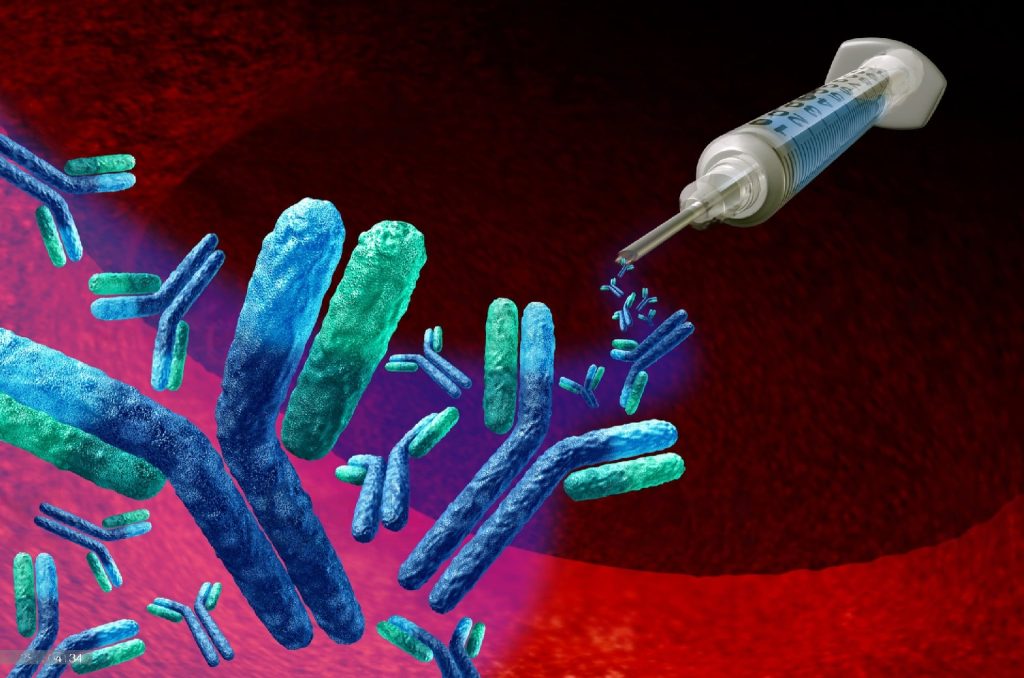
Neutralizing antibodies are antibodies that bind to viruses or other pathogens and prevent them from infecting cells. When a virus enters the body, the immune system responds by producing antibodies. Some of these antibodies can bind to viruses and block them from entering and multiplying in cells, essentially neutralizing them. A neutralizing antibody (NAb) is an antibody that protects cells from pathogens, or organisms that cause sickness. They are naturally created by the body as part of its immune response, and their production is prompted by both infections and anti-infection immunizations.
Neutralizing antibodies play a key role in the immune response to viral infections such as COVID-19. In the instance of COVID-19, neutralizing antibodies attach to and block the virus’s spike protein from binding to and entering cells.
Characteristics:
Neutralizing antibodies have several characteristics that allow them to effectively neutralize a virus or other pathogen. The characteristics of neutralizing antibodies make them a powerful tool in the fight against infectious diseases, as they can effectively prevent and treat infections.
Specificity: Neutralizing antibodies are highly specific for the pathogen they target. They recognize and bind to specific proteins on the surface of the virus or other pathogen.
Affinity: Neutralizing antibodies have a high affinity for the pathogen they target, meaning they bind to it strongly and effectively.
Potency: Neutralizing antibodies are effective at neutralizing the pathogen even at low concentrations.
Cross-reactivity: Some neutralizing antibodies are able to neutralize multiple strains of a virus or even different viruses that share similar proteins or structures.
Durability: Neutralizing antibodies can persist in the body for a period of time after an infection or vaccination, providing ongoing protection against the pathogen.
Functionality: Neutralizing antibodies are capable of preventing the virus from entering cells or replicating within them, effectively stopping the infection process.
Mechanism of production of neutralizing antibodies:
The immune system produces neutralizing antibodies in response to an infection or vaccination. The recognition and activation of immune cells, the production of antibodies that recognize and bind to the pathogen, clonal expansion of B cells, and the generation of memory B cells that can provide long-term protection against the pathogen are all part of the mechanism of neutralizing antibody production. The mechanism of production of neutralizing antibodies involves several steps:
Recognition: When a virus or other pathogen enters the body, it is recognized by the immune system. Specialized cells in the immune system, called antigen-presenting cells, identify the pathogen and display fragments of its proteins, known as antigens, on their surface.
Activation: T cells, another type of immune cell, recognize the displayed antigens and become activated. Activated T cells release cytokines, signaling molecules that help to recruit and activate other immune cells.
Antibody production: B cells, another type of immune cell, are activated by cytokines and begin to produce antibodies that recognize and bind to the antigens displayed on the surface of the pathogen. Some of these antibodies have the ability to neutralize the pathogen by preventing it from entering cells or replicating.
Clonal expansion: Once B cells produce antibodies that recognize the pathogen, they undergo clonal expansion, a process in which they divide and produce a large number of identical cells, or clones, that produce the same antibody.
Memory cells: After the infection is cleared, some of the activated B cells differentiate into memory B cells, which can persist in the body for a long time and quickly respond to future exposure to the same pathogen. Memory B cells can rapidly produce neutralizing antibodies if the pathogen is encountered again, providing long-term protection against the disease.
How neutralizing antibodies work?
The binding of neutralizing antibodies to viral proteins prevents the virus from interacting with host cells, inhibiting replication and causing it to be targeted for destruction by the immune system. This method of action is crucial in avoiding the transmission of infectious diseases and lowering the severity of symptoms in people who are affected.
Neutralizing antibodies work by recognizing and binding to specific proteins on the surface of a virus or other pathogen, preventing it from infecting cells or replicating. The mechanism of action of neutralizing antibodies involves several steps:
Binding: Neutralizing antibodies recognize and bind to specific proteins, known as antigens, on the surface of the pathogen. The antibodies are highly specific for the antigen, meaning they recognize and bind to it with high affinity.
Blocking entry: Some neutralizing antibodies can block the virus from entering cells by binding to the viral protein that interacts with the host cell receptor, preventing the virus from attaching to the host cell.
Direct inactivation: Other neutralizing antibodies can directly inactivate the virus by binding to a protein on the virus and triggering a process that leads to its destruction.
Opsonization: Neutralizing antibodies can also trigger a process known as opsonization, where they coat the surface of the virus and mark it for destruction by immune cells, such as macrophages or natural killer cells.
Factors Affecting the production of Neutralizing Antibody:
The production of neutralizing antibodies is influenced by a range of factors, including the antigenic properties of the pathogen, age, genetics, health status, previous exposure, and vaccination schedule. Understanding these factors is important for optimizing vaccination strategies and developing effective therapies for infectious disease
Antigenic properties of the pathogen: The ability of the immune system to produce neutralizing antibodies is influenced by the antigenic properties of the pathogen. Some pathogens may have antigens that are highly immunogenic, meaning they are highly effective at stimulating the production of neutralizing antibodies, while others may have antigens that are less immunogenic and may require multiple doses of a vaccine to achieve optimal antibody levels.
Age: The production of neutralizing antibodies may decline with age, particularly in older adults. This can lead to reduced protection against certain infections, making vaccination more important for older adults.
Genetics: Genetic factors can influence the production of neutralizing antibodies. Some individuals may have genetic variations that make them more or less susceptible to certain infections or less responsive to certain vaccines.
Health status: Certain medical conditions or medications can weaken the immune system, impairing the production of neutralizing antibodies.
Previous exposure: Prior exposure to a pathogen can influence the production of neutralizing antibodies. In some cases, prior exposure can lead to the development of long-lasting immunity, while in other cases, it may lead to the production of non-neutralizing antibodies that provide limited protection against future infections.
Vaccination schedule: The timing and frequency of vaccinations can affect the production of neutralizing antibodies. In some cases, multiple doses or booster shots may be required to achieve optimal antibody levels.
Clinical Applications:
Neutralizing antibodies have several clinical applications in the prevention and treatment of infectious diseases, and in the development of vaccines. As research into the mechanisms of action and production of neutralizing antibodies continues, new applications for these antibodies may emerge.
passive immunization: Neutralizing antibodies can be used for passive immunization in individuals who have been exposed to a pathogen or who have a weakened immune system. Passive immunization involves the injection of pre-formed antibodies into an individual to provide immediate protection against a pathogen.
Treatment of infectious diseases: Neutralizing antibodies can be used to treat infectious diseases caused by viruses or other pathogens. For example, monoclonal antibodies that target the spike protein of SARS-CoV-2 have been developed as a treatment for COVID-19.
Prevention of infections: Neutralizing antibodies can be used to prevent infections in high-risk individuals, such as healthcare workers or individuals with compromised immune systems. For example, monoclonal antibodies can be used as prophylaxis against HIV infection.
Vaccine development: Neutralizing antibodies are important for the development of vaccines against infectious diseases. By identifying the specific antigens that trigger the production of neutralizing antibodies, vaccines can be developed that stimulate the immune system to produce these antibodies and provide long-term protection against the pathogen.
Test of Neutralizing Antibody:
The test for neutralizing antibodies is called a neutralization assay, and it measures the ability of antibodies to neutralize the infectivity of a pathogen. This test is used to determine whether an individual has produced neutralizing antibodies in response to a vaccine or previous infection.
The neutralization assay typically involves incubating the pathogen with the test serum or purified antibodies in vitro. The mixture is then added to a culture of susceptible cells, and the cells are observed for signs of infection or damage. If the antibodies are able to neutralize the pathogen, there will be no signs of infection or damage to the cells. If the antibodies are not effective, the cells will become infected and show signs of damage.
Neutralization assays can be used to test for neutralizing antibodies against a wide range of pathogens, including viruses, bacteria, and parasites. The assay can also be used to determine the concentration of neutralizing antibodies in a sample, which can be useful for monitoring the immune response to vaccination or treatment.
Overall, the neutralization assay is a valuable tool for measuring the presence and effectiveness of neutralizing antibodies, and for monitoring the immune response to infectious diseases and vaccination.
References:
- Krammer, F. (2020). SARS-CoV-2 vaccines in development. Nature, 586(7830), 516-527.
- Baum, A., Fulton, B. O., Wloga, E., Copin, R., Pascal, K. E., Russo, V., Giordano, S., Lanza, K., Negron, N., Ni, M., Wei, Y., Atwal, G. S., Murphy, A. J., Stahl, N., Yancopoulos, G. D., & Kyratsous, C. A. (2020). Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies. Science, 369(6506), 1014-1018.
- Liu, L., Wang, P., Nair, M. S., Yu, J., Rapp, M. A., Wang, Q., Luo, Y., Chan, J. F.-W., Sahi, V., Figueroa, A., Guo, X. V., Cerutti, G., Bimela, J., Gorman, J., Zhou, T., Chen, Z., Yuen, K.-Y., Kwong, P. D., Sodroski, J. G., & Yin, M.-T. (2020). Potent neutralizing antibodies against multiple epitopes on SARS-CoV-2 spike. Nature, 584(7821), 450-456.
- Brouwer, P. J. M., Caniels, T. G., van der Straten, K., Snitselaar, J. L., Aldon, Y., Bangaru, S., Torres, J. L., Okba, N. M. A., Claireaux, M., Kerster, G., Bentlage, A. E. H., van Haaren, M. M., Guerra, D., Burger, J. A., Schermer, E. E., Verheul, K. D., van der Velde, N., van der Kooi, A., van Schooten, J., … Ward, A. B. (2020). Potent neutralizing antibodies from COVID-19 patients define multiple targets of vulnerability. Science, 369(6504), 643-650.
- Sette, A., & Crotty, S. (2021). Pre-existing immunity to SARS-CoV-2: The knowns and unknowns. Nature Reviews Immunology, 21(8), 457-458.