Introduction to Hepatitis A Virus (HAV):
Hepatitis is the inflammation of liver cells of which viral infection is the most prevalent cause. Hepatitis A, Hepatitis B, Hepatitis C, Hepatitis D and Hepatitis E are the five primary hepatitis viruses.
Hepatitis A virus (HAV), the etiologic agent of viral hepatitis A (infectious hepatitis), is the primary cause of acute viral hepatitis in infants and adults. The prevalence of HAV infection is highest in underdeveloped nations which is attributed to inadequate sanitation.
Morphology and Genome Structure of HAV:
HAV belongs to the Picornaviridae family. HAV is a spherical particle that ranges in size from 27 to 32 nm and has a 7.5 kb linear single-stranded RNA genome. The HAV genome consists of:
- A long 5 Untranslated region (UTR) that has a 2.5 kDa, covalently attached, virus-encoded protein—VPg (also known as 3B)—instead of a cap structure at its 5 terminus.
- A single, large open reading frame (ORF) encoding a polyprotein of about 2,227 amino acids that is proteolytically processed into structural and nonstructural viral polypeptides; and
- A short 3 UTR of 63 nucleotides that is followed by a poly(A) tail of varying lengths (40–80 nucleotides) characteristic of picornavirus genomes.
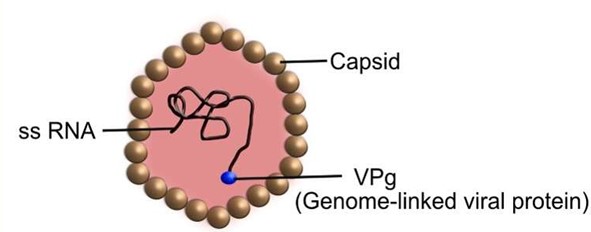
Fig: Morphology of Hepatitis A Virus (HAV)
Transmission and pathogenesis of Hepatitis A Virus:
The virus is excreted in the feces, and HAV is spread feco-orally. The hepatocyte is the primary site of replication. Viral replication causes substantial impairment of liver function.
Following ingestion, viruses travel via the hepatic portal vein from the gastrointestinal tract to the liver. When virions get to the liver, they bind to the hepatocytes’ HAVcr-1 receptors, enter the cells, and multiply there. Following the creation of the virus, its progeny is secreted into the bile canaliculi and liver sinusoids. From there, they are carried to the intestines, where they are ultimately eliminated as feces. Incubation period may range up to 50 days, with a mean of about 30 days. During this time, a short viremia occurs and relatively high amounts of virus are shed in the feces prior to the start of clinical signs. A viremia occurs seven to fourteen days before symptoms appear. Infected individuals typically show no symptoms while the virus is actively replicating. When symptoms do manifest, they are typically nonspecific or minor.
Clinical presentations:
Asymptomatic and Mild Infection
The sickness can range in severity from asymptomatic to anicteric or icteric hepatitis. HAV infections are self-limiting and often resolve on their own in two to four weeks. An infected person may actively excrete the virus in their stool without exhibiting any other signs of illness.
Pre-Icteric (Prodromal) Stage
The second stage, known as pre-icteric, may occur days or weeks before jaundice manifests. Nonspecific symptoms including anorexia, nausea, vomiting, abdominal discomfort, exhaustion, malaise, and fever are indicative of the prodromal stage, myalgia (muscle discomfort), arthralgia (joint pain), pharyngitis, constipation, diarrhea, pruritic (severe itching), and urticaria (itchy skin eruption), hepatomegaly and hepatic discomfort; dark urine due to high bilirubin levels;
Icteric Stage and convalescent Period
The third stage (Icteric stage) presents as characteristic yellowing of the skin and eyes; final stage; convalescent period during which the patient recovers.
Laboratory Diagnosis of HAV:
Sample Collection and Liver Function Tests (LFTs)
The samples for HAV detection can be Serum, liver, bile, stool, and blood.
Clinical, pathologic, and epidemiologic data are supplemented by tests for abnormal liver function, such as serum bilirubin and alanine aminotransferase (ALT). Liver biopsy allows for a tissue diagnosis of hepatitis.
Direct antigen detection
HAV is found in the stool between two weeks before and two weeks after the onset of jaundice. Immunoelectron microscopy has identified virus particles in the fecal extracts of hepatitis A patient; the virus manifests early in the illness and goes away within two weeks after the onset of jaundice.
Serological Diagnosis (IgM, IgG Anti-HAV)
Anti-HAV occurs in the IgM fraction during the acute phase; ELISA is the preferred technique for quantifying HAV antibodies, peaked roughly two weeks following an increase in liver enzymes.
The IgM antibody is the first to show up when symptoms start, and it stays high for one to two months. Within three to six months, anti-HAV IgM often drops to undetectable levels. Anti-HAV IgG manifests shortly after the disease starts and lasts for many years.
Therefore, the diagnosis of hepatitis A is confirmed when IgM-specific anti-HAV is found in the blood of an acutely infected patient.
Molecular diagnosis
Nucleic acid hybridization tests, or PCR can identify HAV in naturally infected persons’ liver, stool, bile, and blood.
