Introduction to Chagas Disease (American Trypanosomiasis):
- American trypanosomiasis is also known as Chagas Disease. It is caused by a flagellated protozoa Trypanosoma cruzi. In endemic regions, different species of three genera of bloodsucking triatomine insects—also referred to as kissing bugs (Triatoma)—transmit T. cruzi.
The mother-to-child transmission rate of T. cruzi is approximately 4.7% (range 3.9–5.6%), and it may be greater in endemic nations compared to non-endemic countries (5% vs. 2.7%). - Additionally, blood and blood products can spread T. cruzi; the estimated transmission rate per infected blood unit is 10–25%. Following solid organ transplantation from an infected donor, kidney patients appear to have reduced infection rates (0–19%) compared to liver recipients (0–29%) and heart recipients (75–100%).
Morphological forms of Trypanosoma cruzi:
Amastigote
Amastigote is small, round, cytoplasmic in shape and is found in the cytoplasm of mammalian host cells. Binary fission separates the flagellum, which is either short or invisible.
Epimastigote
The epimastigote has an elongated shape and a noticeable flagellum. It is present in the triatomine bug’s midgut. It is found and multiplies in the insect’s mitochondrial DNA, or kinetoplast.
Trypomastigote
Trypomastigote is long, thin (12–30 µm) with an undulating membrane and a large kinetoplast.
It is found in mammal bloodstream and vector excrement (infective/metacyclic form). The stage infects new cells or is consumed by insects; it is motile and non-replicative in mammals.
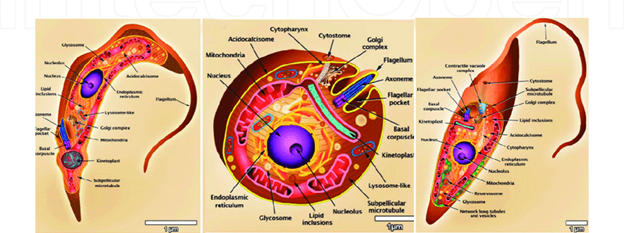
Source: https://www.researchgate.net
Fig: Morphology of T. cruzi (trypomastigote, amastigote, and epimastigote)
Life cycle of T. cruzi:
Both humans and the triatomine (kissing) bug are involved in the life cycle of Trypanosoma cruzi. When the triatomine bug feeds on human blood and excretes feces that contain parasites close to the bite site, infection starts. The bite wound or adjacent mucous membranes, including the eyes, allow the infectious form of the parasite to enter the body. After entering the human host, the parasites transform into amastigotes by invading nearby cells. These forms cause damage to infected tissues by simply dividing within the cells. The amastigotes multiply, then change back into trypomastigotes, break through the host cells, and enter the bloodstream. During a blood meal, circulating trypomastigotes can either infect new cells or be absorbed by another triatomine bug.
The parasites continue to develop inside the insect. Once inside the bug’s midgut, the eaten trypomastigotes transform into epimastigotes and proliferate. After that, they go to the hindgut and change into the human infectious stage, metacyclic trypomastigotes. These parasites complete the cycle and enable transmission to a new human host when they are eliminated in the bug’s feces after a subsequent blood meal.
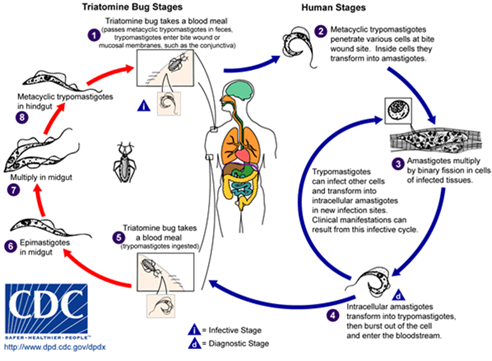
Source: CDC
Fig: Life cycle of T. cruzi
Pathogenesis and Immunological Mechanisms:
Acute phase immune response
In acute Chagas disease, parasite mucins and DNA drive the immune response, and CD8 cells primarily target T. cruzi membrane transsialidases. An imbalance in the T-helper 1 and T-helper 2 response may result in an overabundance of proinflammatory cytokines when the disease progresses to the chronic phase. Through the production of nitric oxide, which has a strong trypanocide effect, the T-helper-1 immune response plays a protective role.
Chronic Chagas disease and cardiomyopathy
To explain chronic Chagas disease cardiomyopathy, four primary pathogenic pathways have been proposed: autonomic nervous system disruption, microvascular abnormalities, and parasite-dependent myocardial manifestations.
Laboratory Diagnosis of Chagas Disease:
Acute infection
For acute vector-borne infection, diagnosis mainly relies on direct detection of the parasite. High levels of parasites can be found in the blood for up to 90 days. This is done by examining fresh blood samples under a microscope, using Giemsa-stained thin or thick blood smears, or the buffy coat technique. Parasite concentration methods, such as the microhaematocrit and Strout techniques, improve detection. Molecular tests like PCR can also be used. Serological tests are not helpful during the acute stage.
Congenital infection
For congenital infection, diagnosis is also based on direct identification of the parasite. Concentration techniques, including the microhaematocrit and Strout methods, are commonly used, and direct microscopy is useful as well. PCR is the most sensitive method for detecting infection. Serological testing becomes reliable only after 9 months of age or later.
Transfusion- and transplant-associated infection
In cases of infection acquired through blood transfusion or organ transplantation, diagnosis also follows the same methods used for vector transmission. However, molecular testing such as PCR often becomes positive days or even weeks before parasites can be seen in blood samples. In certain situations, testing of tissue samples may be required.
Reactivation in immunocompromised individuals
For reactivation in HIV-infected individuals, diagnosis is based on direct identification of the parasite, similar to vector-borne cases. The organism can be detected in cerebrospinal fluid, other body fluids, or tissue samples. PCR is generally not useful for diagnosing reactivation. Serological tests can help confirm chronic infection and are useful when reactivation is suspected.
In reactivation among other immunosuppressed patients, direct parasitological techniques are again used, as in vector-related infection. Parasites may be identified in tissue samples. An increasing parasite load detected by real-time PCR in repeated samples can suggest a high risk of disease reactivation.
