Introduction:
Antibiotics are drugs that eliminate or slow the growth of bacteria, which can cause diseases. In 1942, the term “antibiotic” was coined to characterize any compound produced by a microorganism, and then chemically synthesized, that inhibits the growth of other bacteria. The word is derived from the Greek words ‘anti’ (against) and ‘biotikos’ (concerning life). Antibiotics have saved countless lives and made a variety of medical procedures possible or safer since their introduction. Antibiotics are mostly used to treat bacteria, but they can also be used to treat parasitic infections.
Virus infections are not treated with them. The majority of antibiotics are either natural products extracted from microorganism, semi-synthetically manufactured natural products, or chemically synthesized based on their structure.
History:
Antibiotics have been used to treat infections for millennia, though most people did not realize the infections were caused by bacteria until the last century or so.
Antibacterial compounds were first observed in action in the late 1800s. A German physician named Paul Ehrlich noticed that some bacterial cells were colored by chemical dyes. He discovered that arsphenamine, a chemical, was an excellent therapy for syphilis in 1909. Although Ehrlich referred to his finding as ‘chemotherapy‘ – the employment of a chemical to cure a disease — it became the first modern antibiotic.
The term “antibiotic” had not yet been invented at this time. Ehrlich originated the term chemotherapy to describe the treatment of diseases with chemicals.
New era of antibiotic began with Sir Alexander Fleming’s observation in 1928 concerning the lysis of bacteria on a Penicillium contaminated culture plate left on his workbench. Scientists Ernst Chain and Howard Florey, in 1940, were able to isolate Penicillin. This encouraged researchers to pursue drug development research in the future.
Fleming, Florey, and Chain were awarded the Nobel Prize in 1945 for their contributions to the discovery, research, and development of penicillin.
Most antibiotic families, including aminoglycosides, chloramphenicol, tetracycline, macrolides, rifamycins, and fusidic acid, had representatives discovered by the mid-1950s. Synthetic antimicrobial medications, such as nitroimidazol, quinolones, and most antituberculosis treatments, have been discovered by chemists and microbiologists.
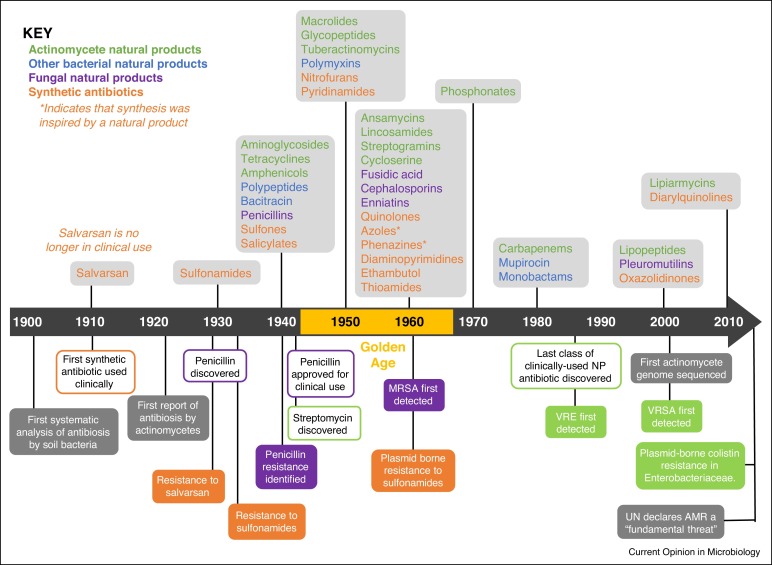
Fig: The introduction of antibiotics into clinical use
Uses:
Antibiotics have always played a crucial role in healing a variety of antibiotic resistances. Many common infectious diseases now have effective therapies.
Antibiotics are a type of antibacterial. The majority of them are commonly given medications that can suppress or even treat bacterial and fungal diseases. It has the potential to stop disease from spreading and to minimize the severity of disease consequences. They are used in both human and farm animal diseases to eliminate bacterial and fungal infections, increase animal weight gain, and limit zoonotic pathogens in milk, egg, meat, and meat products.
Antibiotics are commonly prescribed during:
- Without antibiotics, the infection will persist.
- The infection has progressed to the point where it is creating more serious consequences.
- Without antibiotics, the infection will last far too long.
- Because the condition is highly infectious, it will spread and infect others.
Side Effects:
Antibiotics represents a new age of health-care improvements. Antibiotic overuse and misuse, on the other hand, has led in the emergence of antibiotic-resistant disease strains.
Some of these drugs can be taken orally, while others must be injected intravenously or intramuscularly. Antibiotic toxicity can cause mild side effects like nausea, vomiting, diarrhea, indigestion, abdominal pain, loss of appetite, stomach pain, or cramping; however, more severe side effects that can cause significant morbidity and mortality have been documented for antibiotics like amphotericin B, linezolid, vancomycin, and the azole antifungals.
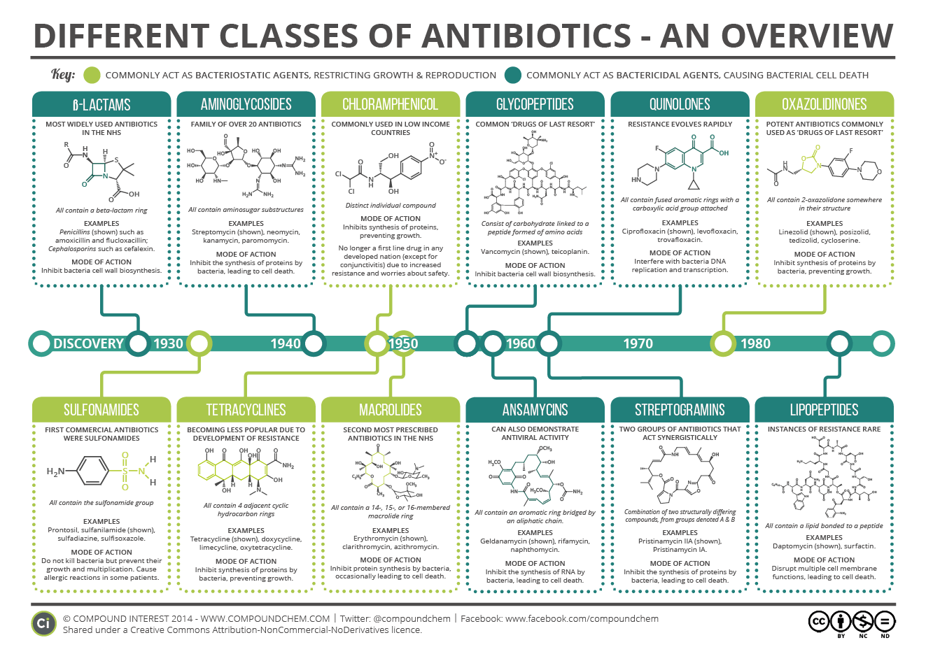
Classification of antibiotics:
Based on the mode of action
- Antibiotics targeting cell wall
- Inhibitors of protein biosynthesis
- Inhibitors of DNA replication
- Folic acid metabolism inhibitors
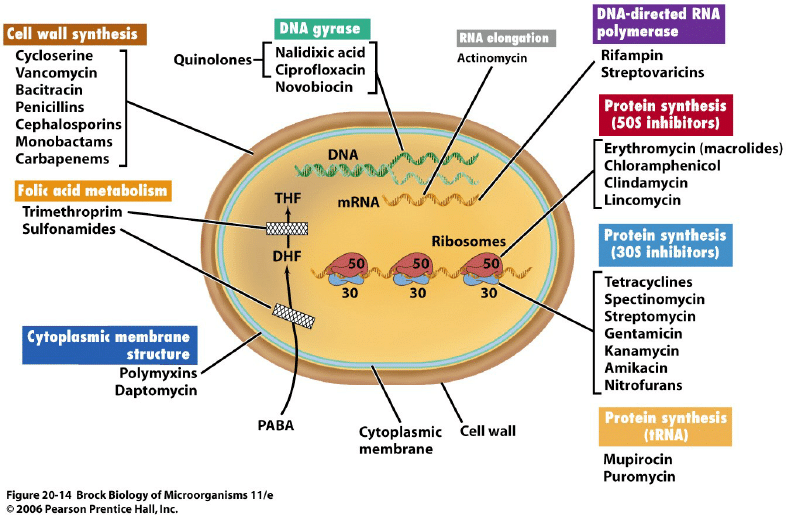
Fig: Mechanism of action of antibiotics
Based on the effects of their activity
1. Bactericidal:
- Kills bacteria
- Examples: Aminoglycosides, Penicillin, Cephalosporin
2. Bacteriostatic:
- Inhibits the growth of bacteria
- Examples: Sulfonamide, tetracycline, chloramphenicol, trimethoprim, macrolides, Lincosamide
Bases on the route of administration
Antibiotics can be given by a number of different routes including by mouth, injection into a vein or by washing inside the uterus and the surgical site with a saline solution containing the antibiotic.
1. Oral antibiotics:
- Acid stable antibiotics,
- Examples; Penicillin V
2. Parenteral route:
- Intravenous administration
- Examples; Penicillin G
Based on spectrum activity (range of activity)
Antibiotics are categorised according to their spectrum of activity, which refers to the variety of bacteria that they are effective against. Broad-spectrum antibiotics can target both Gram-positive and Gram-negative bacteria, but narrow-spectrum antibiotics are only effective against a certain category or species of bacteria.
Based on origin
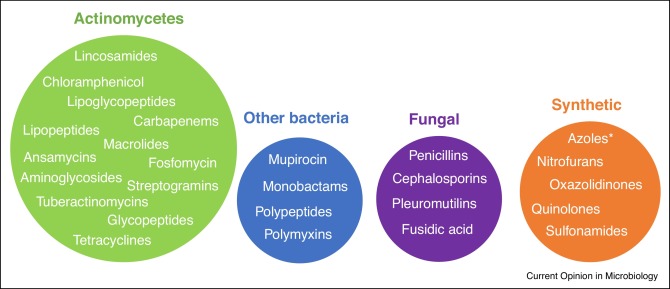
Fig: Most clinically relevant classes of antibiotic are derived from natural products
Antibiotic Resistance:
Antimicrobial resistance (AMR) presents a challenge to the appropriate prevention and treatment of diseases caused by bacteria, parasites, viruses, and fungi, which are becoming more widespread. When a microorganism can grow or survive in the presence of an antibiotic concentration that would normally inhibit or kill organisms of the same species, it is said to be resistant to that antibiotic. Antibiotics, which have revolutionized medicine and saved millions of lives, are under threat due to the rapid growth of resistant bacteria around the world. Microorganisms have become smarter through time, and this, combined with the widespread use of antibiotics in clinical practice, has led in antimicrobial resistance among bacteria.
Some biochemical forms of resistance mechanisms exploited by bacteria include antibiotic inactivation, target change, altered permeability, and pass of the metabolic pathways.
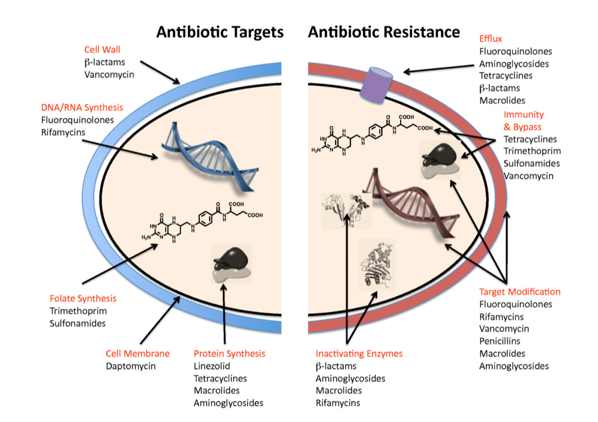
Fig: Mechanism of antibiotic resistance
It is one of the global alarming issues of the 21st century. One of the most serious global challenges of the twenty-first century has been antibiotic resistance. It is beneficial to determine bacterial resistance to antibiotics as well as mutations that cause bacterial resistance to antibiotics. Clinicians will be in highly benefit from a better understanding of the processes of antibiotic resistance as it relates to antibiotic use in various scenarios.
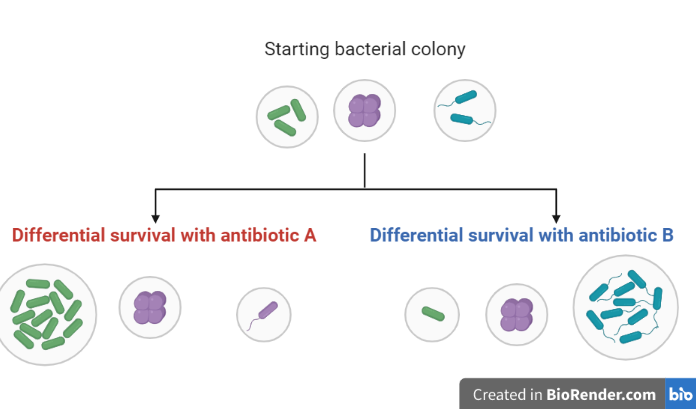
In the developing countries, infections are one of the leading causes of death. This is mostly linked to the appearance of novel infectious pathogens, as well as the emergence of antibiotic resistance. Each year, more than 2.8 million cases of antibiotic-resistant bacterial infections occur, resulting in at least 35,000 fatalities.
Antimicrobial resistance (AMR) across a variety of infectious pathogens is a growing matter of public health that affects many countries and organizations. Governments all across the world are increasingly gaining a better understanding of a severe problem that threatens modern medicine’s achievements.
Antimicrobial Stewardship Programs (ASP):
Antimicrobial stewardship is a coordinated program that encourages the proper use of antimicrobials (including antibiotics), improves patient outcomes, minimizes microbial resistance, and prevents the spread of illnesses caused by multidrug-resistant organisms.
It’s a campaign to track and improve the way clinicians prescribe antibiotics and how patients use them. To successfully treat infections, protect patients from harm caused by inappropriate antibiotic usage, and prevent antibiotic resistance, better antibiotic prescribing and use is crucial.
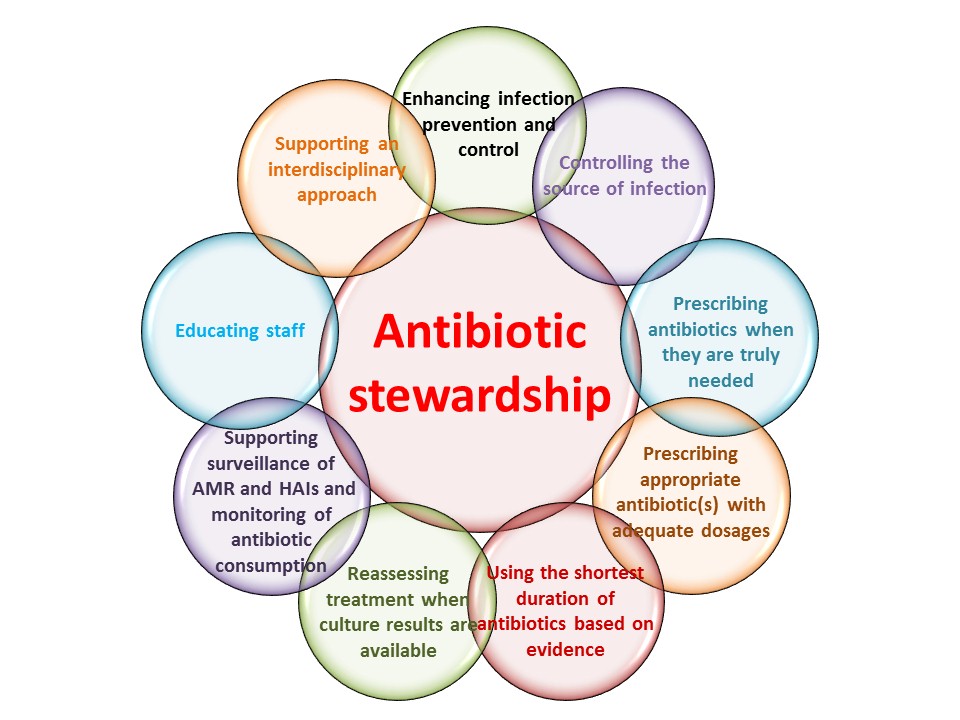
Fig: Aim of the antibiotic Stewardship Program
Future prospects for antibiotic therapy:
Effective antibiotics are essential for future of the modern medicine. Between 1930 and 1962, around twenty new antibiotic classes were developed around the world. Only two additional antibiotic classes have been approved since that time.
During this time period, plenty of analogues of established classes come to the market. Meanwhile, multidrug-resistant bacteria (superbugs) have spread across the globe, and multidrug-resistant bacteria are now responsible for half of all deaths from clinical infection.
The future of medicine is dark if bacteria continue to evolve new resistance mechanisms and the pharmaceutical industry continues to manufacture newer antibiotic classes at the current rate. In our opinion, the industry is unlikely to drastically boost the rate of development of new antibiotic classes. As a result, the current worldwide antibiotic discovery process is likely to be unsustainable in the long term.
Key Points:
- Penicillin, the first natural antibiotic, was discovered by Alexander Fleming in 1928.
- Antibiotics are drugs that are used to treat bacterial infections. Because the symptoms are often extremely similar, differentiating the real cause of infection by bacteria or a virus can be very challenging.
- Antibiotics are ineffective against viral infections.
- Antibiotics either kill or slow bacteria’s growth.
- Diarrhea, stomach distress, and nausea are all possible side effects of antibiotic.
- Antibiotics are most effective when they are used correctly. The first step is to be sure the one absolutely need the antibiotic. Antibiotics should only be used if a bacterial illness has been diagnosed by a doctor.
References:
- Gould K. Antibiotics: from prehistory to the present day. J Antimicrob Chemother. 2016 Mar;71(3):572-5
- COTTER, P.D., HILL, C., ROSS, R.P. (2005). Bacterial lantibiotics: strategies to improve therapeutic potential. Curr Protein Pept Sci. 6, 61-75.
- Hutchings M.I., Truman A.W. and Wilkinson B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80
- Kapoor G, Saigal S, Elongavan A. Action and resistance mechanisms of antibiotics: A guide for clinicians. J Anaesthesiol Clin Pharmacol 2017; 33:300-5.
- Anthony RM Coates, Gerry Halls and Yanmin Hu. Novel classes of antibiotics or more of the same? British Journal of Pharmacology (2011)163184–194.
- Hutchings, M.I., Truman, A.W. and Wilkinson, B., 2019. Antibiotics: past, present and future. Current opinion in microbiology, 51, pp.72-80.
