Introduction:
- Amniocentesis is a medical procedure in which a small sample of the amniotic fluid surrounding a developing fetus is removed and tested.
- The amniotic fluid contains cells shed by the fetus, and the DNA in these cells can be analyzed to determine the genetic makeup of the fetus. Amniocentesis is typically performed during the second trimester of pregnancy, between the 15th and 20th weeks.
- Amniocentesis is usually performed to determine whether a fetus has any genetic abnormalities or conditions that could affect its health. It can be used to diagnose a variety of conditions, including Down syndrome, cystic fibrosis, and neural tube defects. It can also be used to determine the sex of the fetus, although this is not the primary purpose of the procedure.
- Amniocentesis is typically offered to women who are at an increased risk of having a baby with a genetic disorder, such as women who are over 35 years old or have a family history of certain genetic conditions. It is also sometimes offered to women who have had abnormal results on other prenatal tests, such as a first trimester screening test or an abnormal ultrasound.
- It is usually only recommended for women who are at high risk of having a baby with a genetic disorder or who have had abnormal results on other prenatal tests.
Procedure:
Amniocentesis is typically performed between the 15th and 20th weeks of pregnancy. The procedure is usually done in a doctor’s office or clinic, and takes about 15-20 minutes. Here is an overview of the steps involved in an amniocentesis:
Preparation: The patient will be asked to lie on an exam table on the back, with the abdomen exposed. Moreover, the doctor will explain the procedure and may offered a sedative to help relax.
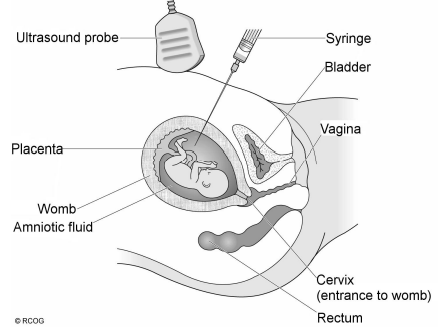
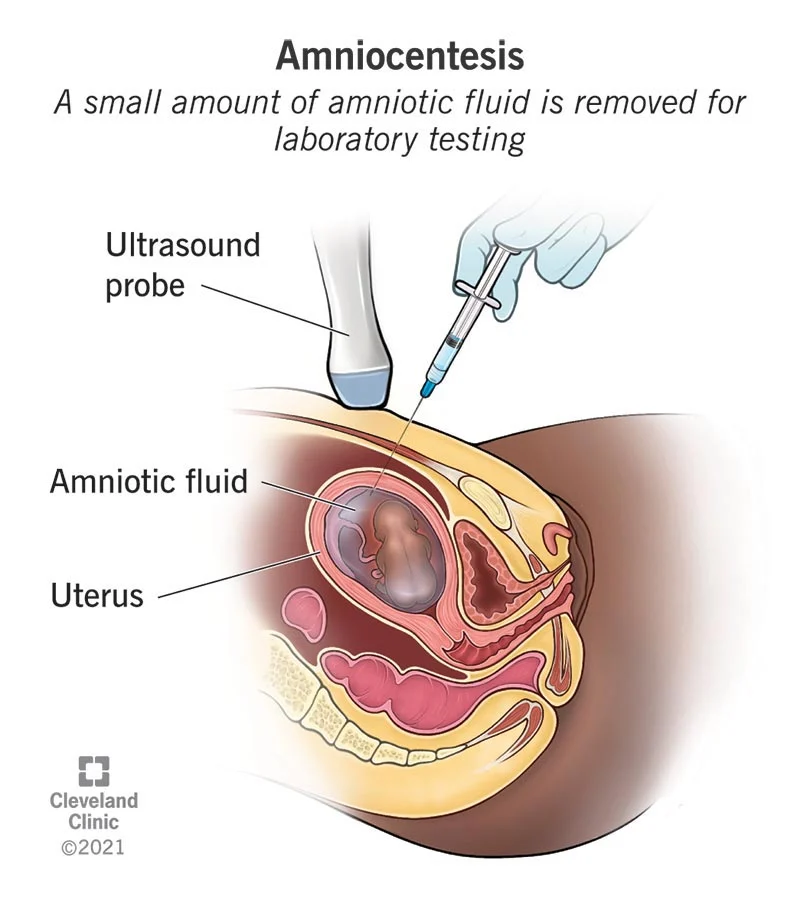
Fig: A procedure of amniocentesis
Ultrasound: The doctor will use ultrasound to locate the fetus and the amniotic sac. Ultrasound uses sound waves to create a image of the inside of your uterus, which helps the doctor to guide the needle to the correct location.
Needle insertion: Using a thin needle, your doctor will insert the needle through the abdomen and into the uterus. The needle will be guided through the uterus and into the amniotic sac using ultrasound.
Amniotic fluid sampling: Once the needle is in the correct location, a small amount of amniotic fluid will be drawn into a syringe. The fluid will be sent to a laboratory for genetic testing.
After the procedure: Once the procedure is complete, the needle will be removed and a bandage will be placed over the site where the needle was inserted. The patient will be asked to rest for a short period of time before going home.
Most women report only mild discomfort during the procedure, and any discomfort should go away shortly after the procedure is complete. One may experience some mild cramping or spotting for a few days after the procedure. It’s important to follow the doctor’s instructions for post-procedure care, including avoiding strenuous activity for a few days.
Benefits:
The amniotic fluid contains cells shed by the fetus, which can be used for genetic testing to identify certain chromosomal abnormalities or genetic disorders in the fetus. There are several benefits to having an amniocentesis, including:
Early diagnosis: Amniocentesis can be performed as early as the 15th week of pregnancy, allowing for early diagnosis of certain genetic disorders. This can help parents to make informed decisions about the pregnancy and their options.
Accurate results: Amniocentesis is considered to be the most accurate method of genetic testing during pregnancy. It has a high accuracy rate for identifying genetic disorders, such as Down syndrome, trisomy 18, and neural tube defects.
Peace of mind: Amniocentesis can provide expectant parents with peace of mind by giving them accurate information about the health of their baby. This can help parents to make informed decisions about the pregnancy and their options.
Treatment options: If a genetic disorder is detected through amniocentesis, parents may have the option to seek treatment for the disorder before the baby is born. This can help to improve the chances of a healthy outcome for the baby.
What does amniocentesis test for?
It’s important to note that amniocentesis is not a comprehensive genetic screening test and does not test for all possible genetic disorders. Amniocentesis can test for a wide range of genetic disorders, including:
Chromosomal abnormalities: Amniocentesis can detect chromosomal abnormalities, such as Down syndrome (trisomy 21), trisomy 18, and trisomy 13. These chromosomal abnormalities can cause physical and cognitive disabilities in affected individuals.
Neural tube defects: Amniocentesis can also detect neural tube defects, such as spina bifida, which is a birth defect that affects the spinal cord.
Genetic disorders: Amniocentesis can detect genetic disorders, such as sickle cell anemia and Tay-Sachs disease.
Sex-linked disorders: Amniocentesis can also detect sex-linked disorders, such as hemophilia, which is a blood clotting disorder that affects males.
Risks:
It’s important to discuss the risks and benefits of amniocentesis with the doctor before deciding whether to have the procedure. The doctor will be able to help discuss the potential risks against the potential benefits and determine if amniocentesis is the right choice for the individual patient. Amniocentesis is generally considered to be a safe procedure, although there is a small risk of complications. The most common complications of amniocentesis include:
Infection: There is a very small risk of infection at the site where the needle was inserted. This risk can be reduced by following proper sterilization techniques.
Bleeding: There is a small risk of bleeding at the site where the needle was inserted.
Injury to the fetus: There is a very small risk of injury to the fetus during the procedure. This risk can be minimized by using ultrasound to guide the needle to the correct location.
Loss of pregnancy: In very rare cases, amniocentesis can cause a miscarriage. This risk is estimated to be about 1 in 300-400 procedures.
Alternative Testing Options:
Non-Invasive Prenatal Testing (NIPT)
Chorionic Villus Sampling (CVS)
Other Genetic Testing Methods
Preimplantation Genetic Testing (PGT)
Carrier Testing
References:
- http://www.geneticalliance.org.uk/services.htm
- The Royal Women’s Hospital Fact Sheet / www.thewomens.org.au
- Nizard J. Amniocentesis: technique and education. Curr Opin Obstet Gynecol. 2010 Apr;22(2):152-4.
- Smidt-Jensen S, Sundberg K. Early amniocentesis. Curr Opin Obstet Gynecol. 1995 Apr;7(2):117-21.
- Alfirevic Z, Sundberg K, Brigham S. Amniocentesis and chorionic villus sampling for prenatal diagnosis. Cochrane Database Syst Rev. 2003;(3):CD003252.