Introduction:
Cancer is a broad term for a group of disorders characterized by abnormal cell proliferation with the potential to invade or spread to other parts of the body. It is developed as a result of mutations, or aberrant alterations, in the genes that regulate the proper growth and development of the cell.
Breast cancer is caused by the uncontrollable proliferation of breast cells. It occurs when breast cells mutate and proliferate uncontrollably, resulting in a mass of tissue called tumour. Breast cancer, like other cancers, can invade and grow into the tissue surrounding the breast. It can also spread to other parts of your body and produce new tumours, a process known as metastasis.
A tumour is a cluster of abnormal cells. Depending on the types of cells in a tumour, it can be:
- Benign: The tumour doesn’t contain cancerous cells with distinct, smooth, regular borders. A benign tumour can become quite large, but it will not invade nearby tissue or spread to other parts of your body
- Premalignant or precancerous: It contains abnormal cells with the potential to develop into malignant tumours.
- Malignant: A malignant contain cancerous cell which has irregular borders and grows faster than a benign tumour. If untreated, malignant cells eventually can spread
beyond the original tumour to the other parts of the body.
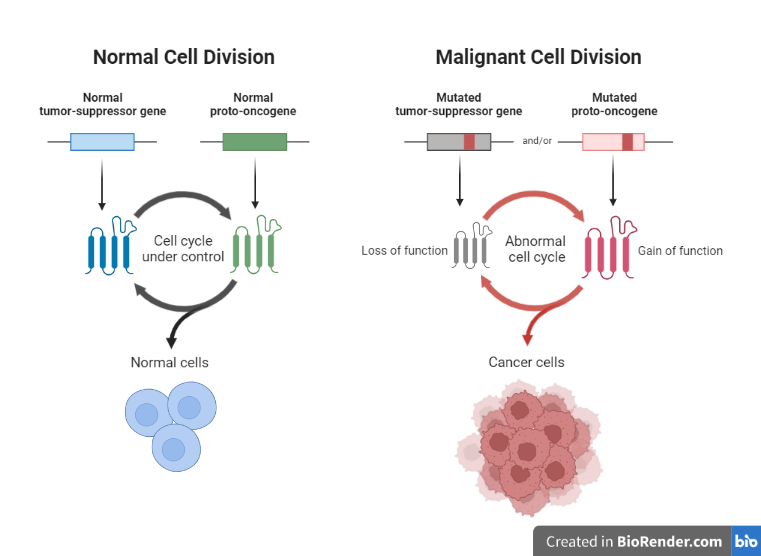
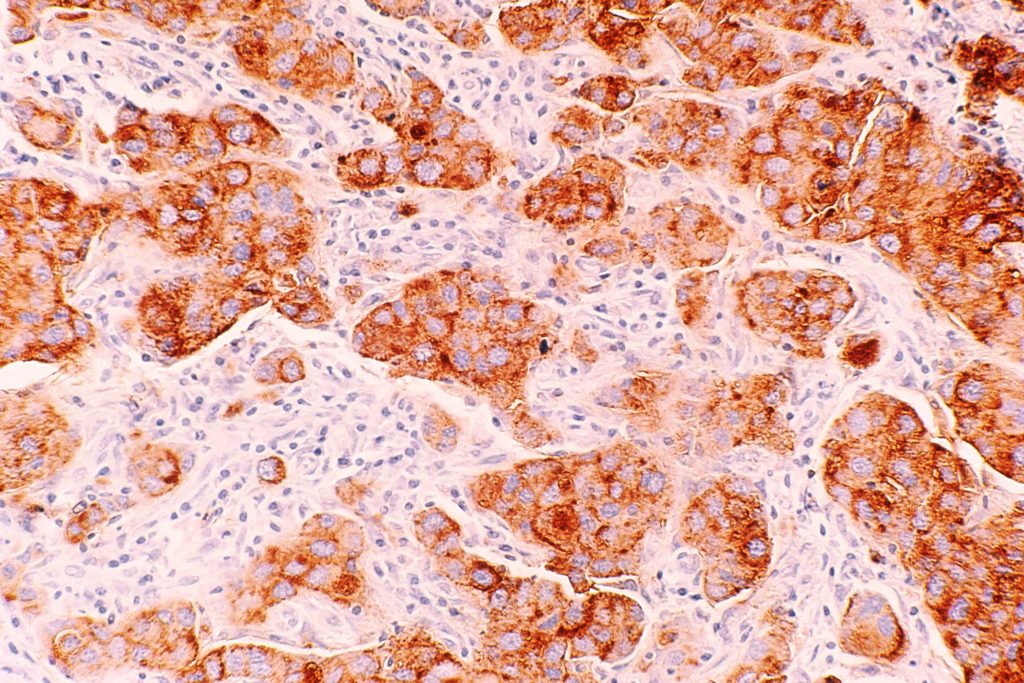
Fig: Normal cell vs cancer cells
There are various types of breast cancer which is determined by which cells in the breast that is developed into cancer. It can be initiated from any area of the breast.
Lobules, ducts and connective tissue are the major components of a breast with their individual functional. The lobules are the milk-producing glands. While, the ducts act as a tube that help in transportation of milk to the nipple. The connective tissue which includes fibrous and fatty tissue surrounds and binds all the parts in together.
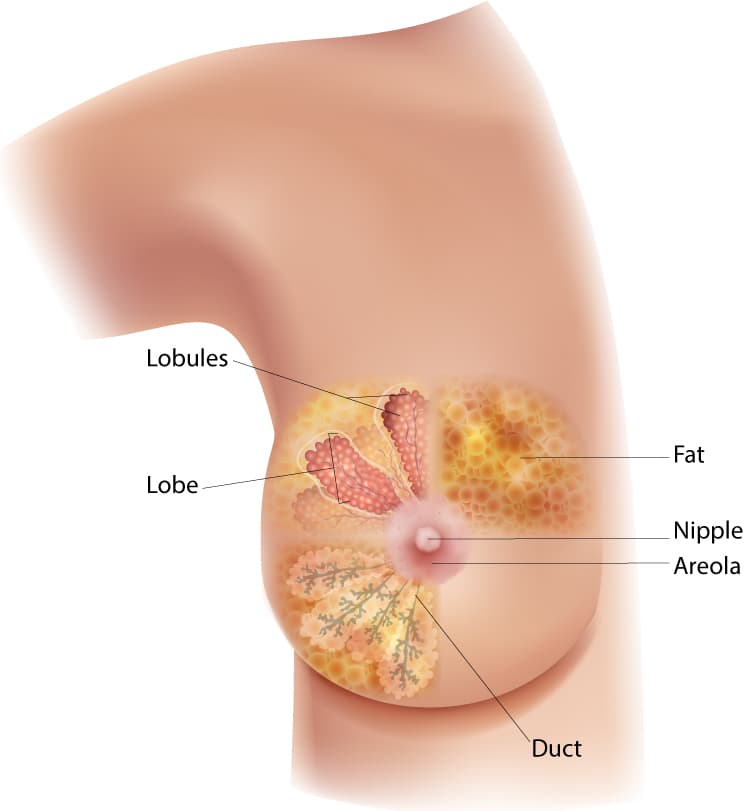
Fig: The diagram of the breast showing the location of the lobules, lobe, duct, areola, nipple, and fat.
Ducts or lobules always stand as a starting point for the majority of the breast cancer which is then spread outside of the breast via blood and lymph arteries which is known as metastasis.
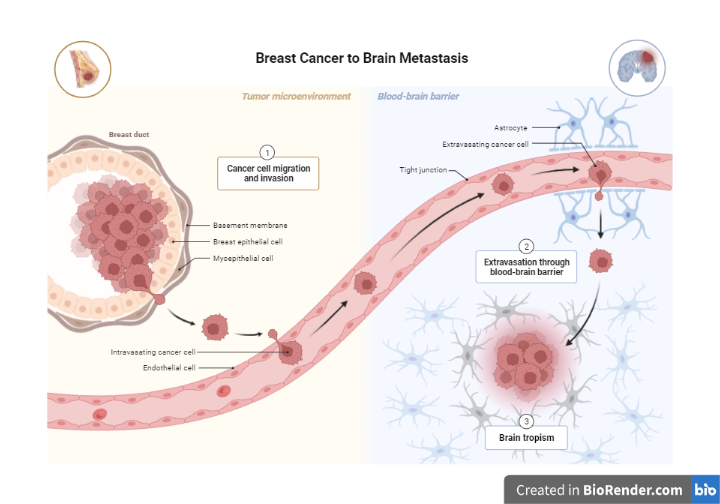
Fig: Metastasis of breast cancer
Incidence:
Breast cancer, second only to skin cancer, is one of the most frequent cancers among women. Women over the age of 50 are most likely to be impacted. Women are mor prone to breast cancer than men.
Since 2007, the rate of breast cancer has remained the same in women under 50. However, have continued to decline in older women. The death rate decreased by 1% every year from 2013 to 2018. Earlier detection of breast cancer through screening and increased awareness, as well as improved treatment options have played a crucial role in the reduction of its rate
Breast cancer rates differ tremendously by nation, with the greatest rates in the United States and Northern Europe and the lowest rates in Asia. In the United States, the average probability of a woman getting breast cancer at some point in her life is around 13%. This means she has a 1 in 8 probability of developing breast cancer.
Breast cancer is diagnosed in around 264,000 women and 2,400 males in the United States each year. Breast cancer kills about 42,000 women and 500 men in the United States each year. Breast cancer caused the death of Black women at a higher rate in comparison to white women.
Symptoms:
In the early stages of breast cancer, there is no pain or discomfort. It can cause a lump or thickening in or near the breast or underarm area, as well as a change in the size or appearance of the breast, nipple discharge or soreness, and swelling, redness, or scaling of the breast, areola, or nipple skin.
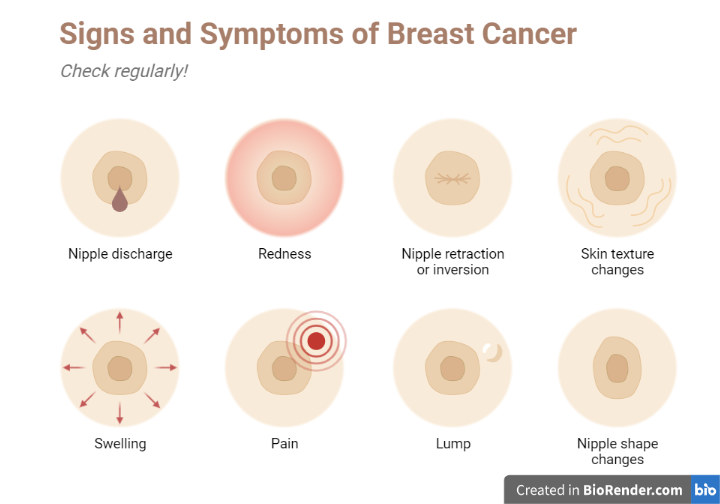
Fig: Sign and symptoms of breast cancer
Causes of disease:
Early menarche (before the age of 12), late natural menopause (after the age of 55), not bearing children, first pregnancy after the age of 30, ionising radiation exposure from medical treatment such as X-rays – particularly during puberty, and hormone therapy are all associated with an increased risk of breast cancer in women.
Several factors are responsible for the causes
Pregnancy-related and hormone-related factors
The exposure to hormones (endogenous estrogen and progesterone) produced by the ovaries has been associated to a woman’s risk of developing breast cancer, according to studies. Breast cancer risk has been connected to reproductive factors that increase the duration and/or intensity of ovarian hormone exposure, which stimulates cell growth. Early menstruation, late menopause, and factors (later age at first pregnancy and never having given birth) allow breast tissue to be exposed to high levels of hormones for longer periods of time.
Anthropometric indices and physical activity:
Breast cancer risk is linked to height, weight, and BMI. BMI and breast cancer risk are linked in both pre- and postmenopausal women, but the correlation is stronger in postmenopausal women.
Environmental exposures
Breast cancer risk is increased when people are exposed to pollutants in the environment. The level of risk associated with environmental pollutants varies based on the amount and type of exposure, as well as the time of exposure and the components of each pollutant.
Tobacco smoke (both active and passive exposure), food (e.g., charred and processed meats), alcohol intake, and environmental carcinogens (e.g., pesticides, radiation, and environmental and dietary estrogens) are only a few of the factors that contribute to the development of breast cancer.
Dietary factors
Overweight or obesity, which is a risk factor for breast cancer, can result from high-fat diets. Because excess fat cells produce estrogen, which can stimulate increased breast cell growth, obese women are thought to be at a higher risk for breast cancer. Breast cancer is more likely as a result of this additional growth.
Consumption of red meat, animal fats, and refined carbs has been connected to a higher risk of breast cancer, but consumption of fruits, vegetables, whole grains, and dietary fibre has been linked to a decreased risk.
Stages of Breast cancer:
The characteristics of a breast cancer, such as its size and whether or not it includes hormone receptors, determine the tumour’s stage.
The cancer stage will help health care professionals determine the prognosis, the expected outcome of breast cancer treatment, and, ultimately, the best treatment options.
Breast cancer stage is commonly indicated as a number on a range of 0 to IV, with stage 0 referring to non-invasive tumours that remain in their original position and stage IV referring to invasive tumours that have moved outside the breast to other areas of the body.
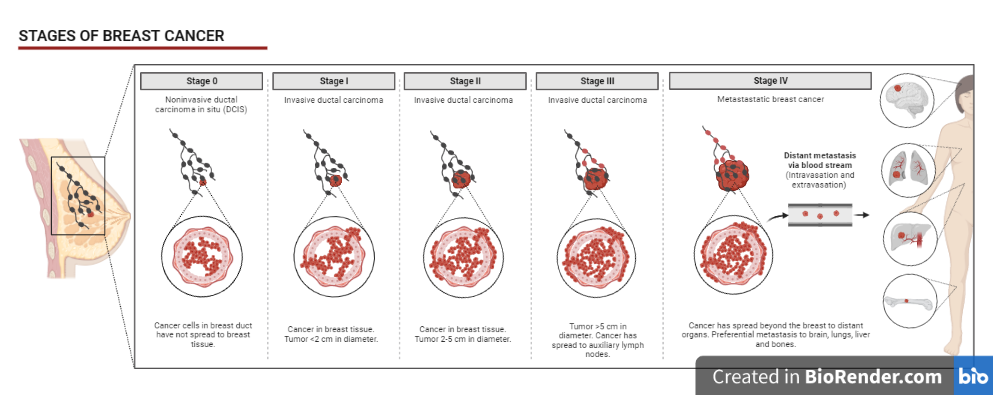
Fig: Stages of breast cancer
Risk factors in breast cancer:
Some features make a person more likely to get breast cancer are called risk factors. Some risk factors are in your control while other are beyond our control.
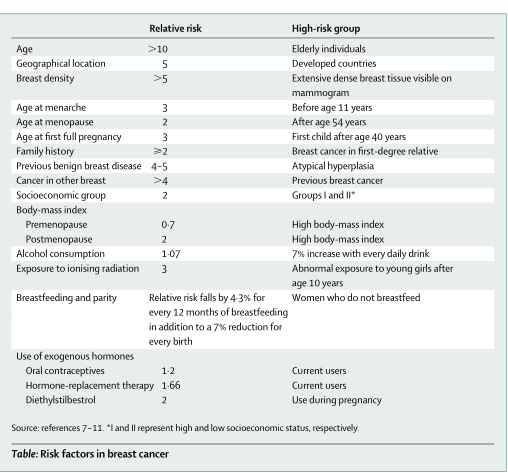
Fig: Several risks factors associated with breast cancer
Molecular Basis
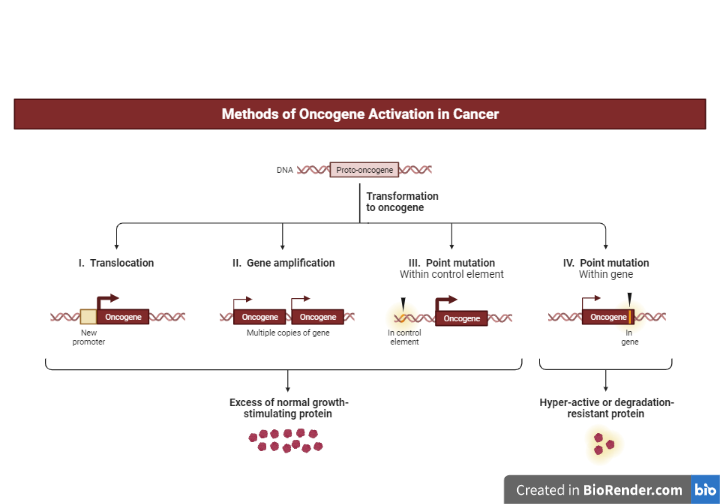
Genes are all in responsible of how our cells work. They are made up of DNA, a molecule that comes from both of our parents. DNA has an impact on more than simply our appearance; it can also influence our risk of developing certain diseases, including cancer.
Proto-oncogenes are genes found in normal cells that help control when they grow, divide to form new cells, or stay alive. A proto-oncogene becomes an oncogene when it is mutated (changed) in a specific way. These mutant oncogenes can cause cancer in cells.
Tumour suppressor genes are also found in regular cells, and they help regulate how often normal cells split in two, and repair in case of any DNA errors. However, the cell can turn in to cancer if there will any mutation in tumour suppressor gene.
Gene alterations that turn on oncogenes or turn down tumour suppressor genes can cause cancer. Breast cancer is generally triggered by changes in a variety of genes.
BRCA gene
A total of 30% of hereditary breast cancer (HBC) are caused by the BRCA1 and BRCA2 genes globally.
Breast cancer can be linked to known gene mutations inherited from one’s mother or father in about 5-10% of cases.
Women with the BRCA1 mutation had a 72% lifetime risk of developing breast cancer. The risk is 69 % for women who have a BRCA2 mutation. Breast cancer in women who have the BRCA1 or BRCA2 mutations is more common in younger women. Moreover, ovarian cancer is also connected to these genetic changes. BRCA2 mutations are linked to a 6.8% lifetime risk of breast cancer in men; BRCA1 mutations are a less common cause of breast cancer in men.
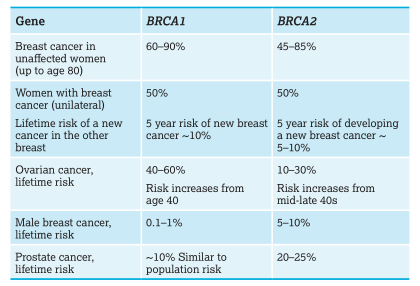
Fig: Risks associated with BRCA1 and BRCA2 gene
Human Epidermal Growth Factor Receptor (HER)
EGFR or HER1, HER2, HER3, and HER4 are members of the human epidermal growth factor receptor (HER) family that promotes cell proliferation, differentiation, migration, and survival. Many types of malignancies are linked to overexpression or improper activation of HER1-3 HER1-3 are associated with their start, development, migration, and invasive features of several types of cancer. HER2 is also a well-known target for a number of malignancies, including breast cancer.
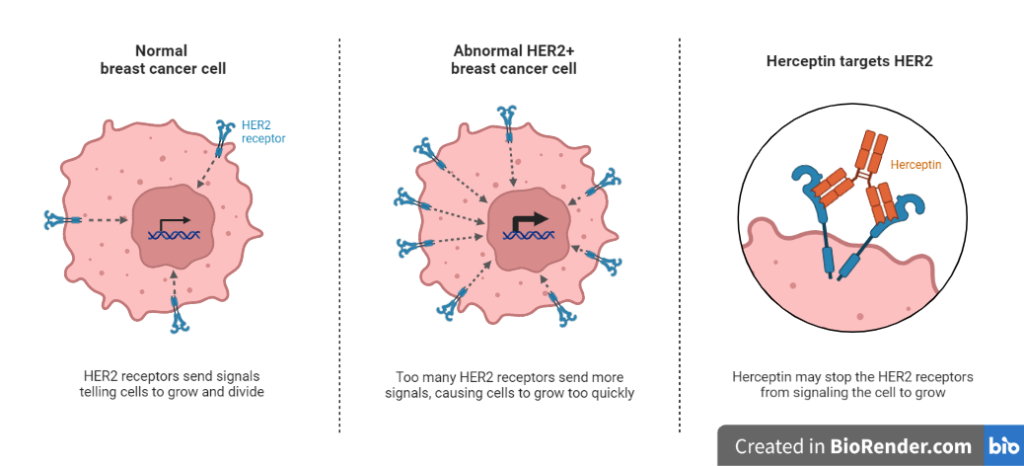
Fig: Molecular basis of HER gene
Estrogen metabolism
Estrogen homeostasis is critical for a wide range of physiological activities, including energy metabolism regulation and sexual development. A growing body of evidence demonstrates that when estrogen equilibrium is disrupted, inappropriate estrogen buildup is a pivotal part in breast cancer development.
Diagnostic procedures:
Mammography, ultrasonography, MRI, and PET are all prominent procedures used to diagnose breast cancer. Physical examination is still crucial because a small percentage of breast cancers (11%) are not detected by mammography.
In women with dense breast tissue, mammography remains the most significant diagnostic tool. Mammography is usually the best way to find small, non-palpable lesions after menopause. Ultrasonography, on the other hand, is the most effective method for detecting tiny tumours in women with dense breasts and distinguishing solid lesions from cystic lesions.
These tests may include:
Ultrasonography
Sound waves are used to take photographs of the tissues inside your breast in this exam. It’s utilized to figure out if there are any lumps or abnormalities in the breast.
Mammogram
These special X-ray images can detect changes or abnormal growths in your breast. Breast cancer prevention frequently involves the use of a mammogram.
Magnetic resonance imaging (MRI)
Magnets and radio waves are used in this test to provide clear, detailed photographs of the structures inside the breast. Health personal may conduct a biopsy of the breast tissue if the imaging tests reveal anything abnormal. The biopsy sample will be sent to a pathology lab for analysis.
Positron emission tomography (PET) scanning
Special dyes are used in PET scans to identify the suspicious locations. Specific dyes will be injected into the veins and images will be taken form the scanner.
Prevention:
Breast cancer cannot be completely avoided. However, there are several precautions that can be applied to minimize the danger. This is especially beneficial for women who have certain breast cancer risk factors, such as a significant family history or certain hereditary gene alterations.
- Limit alcohol
- Maintain a healthy weight.
- Limit postmenopausal hormone replacement therapy.
- Breast-feed.
- Be physically active.
- Lose excess weight
- Follow a healthy eating pattern

Fig: Prevention of cancer
Treatment:
The main treatments for breast cancer are:
References:
- Colditz GA, Baer HJ, Tamimi RM. Breast cancer. In: Schottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
- Xiao, Y., Xia, J., Li, L. et al. Associations between dietary patterns and the risk of breast cancer: a systematic review and meta-analysis of observational studies. Breast Cancer Res 21, 16, 2019
- Cai Xiaoqing, Zhang Libing, Chen Shengxi. Cancer Treatment and Early Detection Targeting HER Receptors. Frontiers in Molecular Biosciences. Vol 9, 2022.
- Santen RJ, Stuenkel CA, Yue W. Mechanistic Effects of Estrogens on Breast Cancer. Cancer J. 2022 May-Jun 01;28(3):224-240.
- Chappuis, Pierre O., Victoria Nethercot, and William D. Foulkes. “Clinico–pathological characteristics of BRCA1‐and BRCA2‐related breast cancer.” In Seminars in surgical oncology, vol. 18, no. 4, pp. 287-295. New York: John Wiley & Sons, Inc., 2000.