Introduction:
Inflammation is a normal response of the living tissue to protect tissues from injury, infection, or diseases that bring cells and molecules of host defense to the sites in order to eliminate causative agents and restore tissue to normality. It is a part of innate immunity, a protective response of the living system.
The event triggered the synthesis and release of the chemical agents by the infected, injured or diseased tissue which eventually developed clinical presentation such as redness, swelling, pain, heat and loss of function. Moreover, the infected tissues may generate additional signals that recruit leukocytes to the site of inflammation which destroy the causative agent, and remove cellular debris from damaged tissue. Normally, this inflammatory response aids in healing, but if uncontrolled, it can become hazardous.
Causes:
- Pathogens such as viruses, fungi, bacteria, parasites.
- Physical agents like radiation, toxic substances, chemicals.
- Diseases or medical condition also may cause inflammation such as Cystitis, bronchitis, dermatitis, autoimmune diseases (Rheumatoid Arthritis, multiple Sclerosis, systemic lupus Erythematosus), Sepsis, cancer
- Immunological injury (AIDS)
- Trauma, Fractures, external burn
- Tissue necrosis
Components of inflammation:
Many immune cells, tissues, molecular mediators, and blood vessels are involved in the inflammatory reaction, including
- Plasma fluid proteins such as clotting systems that help to stop bleeding by forming clot.
- Circulating leukocytes such as neutrophils, monocytes, eosinophils, lymphocytes, basophils, in addition to platelets.
- Blood arteries to improve blood flow to the injured area.
- Macrophages, lymphocytes, fibroblasts, and mast cells are the cells that make up connective tissue.
- Mediators such as histamine, serotonin, bradykinin, fibrinopeptides in order to increase the vascular permeability and contraction of smooth muscle.
- The extracellular matrix consists of structural proteins (collagen, elastin), adhesive glycoproteins (fibronectin, laminin), and proteoglycans that play a major role in fibrosis and tissue repair.
Sign:
- Rubor (Redness)
- Calor (Warmth, Heat)
- Dolor (pain)
- Tumor (Swelling)
- Loss of function
- Fever (pyrexia)
- Vomiting, fatigue, skin rash
Steps of inflammation:
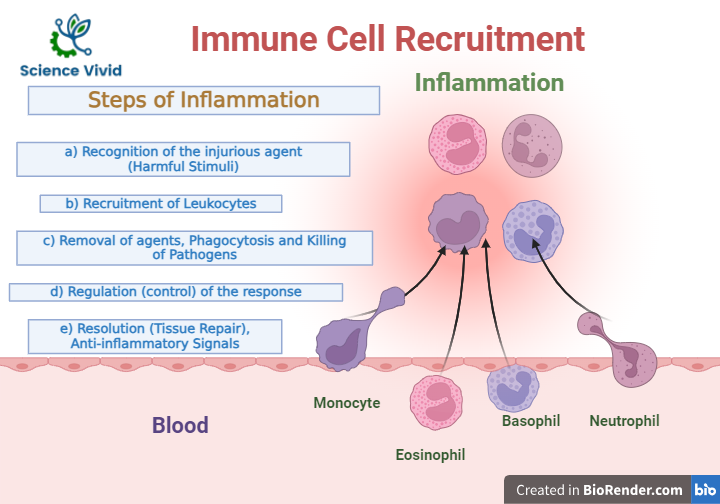
Fig: Steps of inflammation
Types of inflammation:
Acute inflammation
Acute inflammation typically lasts only a few days. If an area of infection turns red, hot, hurts, and swells, it symbolizes that inflammation is at work. In this instance, inflammation is a beneficial process, serving to immobilize the area of injury as the rest of the immune system mobilizes to heal and repair.
Acute inflammation is the initial line of defense which is a rapid response to an injurious agent, injury, or infection. It serves to recruit and deliver mediators of host defense including leukocytes, monocytes, macrophages and plasma proteins to the site of damage within 24-48 hours.
The treatment of acute inflammation includes the administration of aspirin and other non-steroidal anti-inflammatory agents that provides relief of pain and fever for patients.
A) Vascular events
- Transient vasoconstriction
- Vasodilation
- Increase vascular permeability is a hallmark feature of acute inflammation.
B) Cellular events
Accumulation of leukocytes in the periphery of lumen and leucocyte adhere transiently to endothelium. Extravasated WBCs emigrate unidirectionally toward the site of injury.
Chronic inflammation
Chronic inflammation is slow, long-term inflammation, persistent injury, lasting for prolonged periods (months to years), even indefinite, and may become the problem rather than the solution to infection, injury or disease.
Tissues that are chronically inflammatory continue to generate signals that attract leukocytes from the bloodstream into the tissue which will amplify the inflammatory response.
This chronic inflammatory response can break down healthy tissue resulting in tissue necrosis and fibrosis in a misdirected attempt at repair, healing, and maintaining homeostasis.
Chronic inflammation is characterized by
- Main cells are- mononuclear cells (macrophages/monocytes/ lymphocytes/ plasma cells)
- Local signs and symptoms are not prominent.
- Tissue destruction is the hallmark of chronic inflammation.
- Pro-inflammatory cytokines are IL1, IL6, TNF-alpha
Inflammations don’t always help the body. Certain illnesses result in the immune system unintentionally attacking the body’s own cells, which can lead to dangerous inflammations. Atherosclerosis, heart disease, Alzheimer’s disease, rheumatoid arthritis (RA), cancer, multiple sclerosis (MS), diabetes, infections (bacteria, fungi, parasites), inflammatory bowel diseases like Crohn’s disease or ulcerative colitis, gout, inflammatory bowel disease (IBD), aging, congestive heart failure (CHF), and psoriasis (a chronic skin disease) are among the degenerative diseases that are more likely to develop as a result of persistent chronic inflammation.
