Introduction:
Preimplantation Genetic Screening (PGS) is a laboratory procedure that is performed on embryos during in-vitro fertilization (IVF) to determine if they have the correct number of chromosomes (aneuploidy) before they are implanted into the uterus. This test can help identify embryos that have a higher chance of implanting successfully and resulting in a healthy pregnancy. PGS is also known as PGT-A, preimplantation genetic testing for aneuploidies.
PGS can also be used to screen for specific genetic conditions, such as cystic fibrosis or Tay-Sachs disease, if a couple is known to be at risk for those conditions. It is important to note that PGS is not 100% accurate and that further genetic testing may be necessary during pregnancy.
Evolution:
The evolution of PGS has seen an increase in accuracy and the ability to test for a wider range of genetic disorders. Initially, PGS was only able to detect chromosomal abnormalities, but now it is possible to test for specific genetic disorders such as cystic fibrosis and sickle cell anemia. Additionally, the development of next-generation sequencing (NGS) technology has greatly improved the accuracy of PGS and has made it possible to test for even more genetic conditions.
Technology:
Depending on the specific application and the genetic conditions being tested for, different technologies may be used in combination to provide a comprehensive analysis of an embryo’s genetic makeup.
- Fluorescence in situ hybridization (FISH): This technique uses fluorescent probes to detect specific chromosomes or genetic regions. It is often used to detect chromosomal abnormalities such as Down syndrome.
- Polymerase chain reaction (PCR): This technique amplifies specific genetic regions, making it possible to detect small amounts of genetic material. PCR is often used to detect specific genetic disorders such as cystic fibrosis and sickle cell anemia.
- Comparative genomic hybridization (CGH): This technique compares the genetic material of an embryo to a reference genome, allowing for the detection of chromosomal abnormalities.
- Array-based comparative genomic hybridization (aCGH): This technology allows to detect chromosomal abnormalities and also can be used for aneuploidy screening.
- Next-generation sequencing (NGS): This technology allows for the simultaneous analysis of multiple genetic regions, providing a more comprehensive view of an embryo’s genome. It is considered more accurate, efficient, and cost-effective than previous techniques.
Who should get PGS testing?
Preimplantation Genetic Screening (PGS) is typically recommended for couples who have a history of recurrent miscarriage or failed IVF cycles, couples who are at an advanced age, or couples who have a known genetic condition that they wish to screen for. PGS can also be used to screen for chromosomal abnormalities, which can occur in any pregnancy, but are more common in women over 35. PGS testing may also be recommended for individuals who have a family history of genetic disorders, or for couples who have undergone a pre-implantation genetic diagnosis (PGD) for a specific genetic disorder. It is important to note that PGS is not recommended for everyone and the decision to undergo PGS testing should be made in consultation with a qualified reproductive endocrinologist or genetic counsellor.
- Advanced maternal age-As a woman gets older, the chances of chromosomal abnormalities in her eggs increase, so PGS may be recommended for women over 35 years of age.
- History of recurrent miscarriage-PGS may be recommended for couples who have had recurrent miscarriages, as chromosomal abnormalities may be a contributing factor.
- Family history of genetic disorders-PGS can also be used to screen for specific genetic disorders that run in a family.
- Failure of previous IVF cycles-PGS may be recommended if a couple has had multiple failed IVF cycles, as chromosomal abnormalities in the embryos may be a contributing factor.
Why PGS testing should be done?
- To determine the presence or absence of specific genetic conditions in embryos before implantation
- To identify genetic disorders in early pregnancy
- To help couples who are at a higher risk of passing on inherited genetic disorders to their children
- To assist with family planning and the selection of embryos with the desired genetic characteristics
- To guide prenatal care and management of the pregnancy
- To inform decisions about termination of pregnancy
- To provide information for preimplantation genetic diagnosis (PGD) for couples undergoing in vitro fertilization (IVF)
Procedure of PGS testing:
PGS (Preimplantation Genetic Screening) is a genetic test that can be performed on embryos created through in vitro fertilization (IVF) before they are implanted into the uterus.
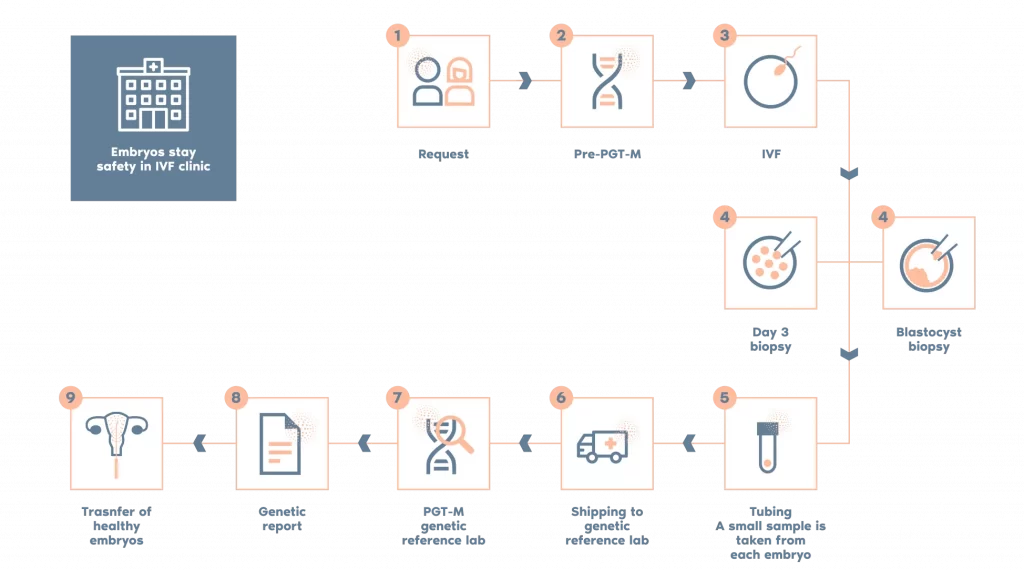
Fig: Procedure of PGS testing
- A small sample of cells (usually 3-5) is taken from each embryo at the 8-cell stage of development. The sample collection process is performed under microscope guidance, by trained embryologists and/or geneticists.
PGS can be performed at various stages, either on oocytes or embryos. Normally it will be performed at day 5 (blastocyst) stage, this will be discussed with you by your doctor and at your consultation with one of our embryologists.
Approximately 5-10 cells are removed from the blastocyst in a technique called biopsy. The biopsied cells were cleaned and transferred to a PCR tube containing 2.5 uL of phosphate-buffered saline (PBS), the embryos will then be cryopreserved (frozen) and stored.
- The cells are analyzed for chromosomal abnormalities using a technique called array CGH (comparative genomic hybridization) or Next-generation sequencing (NGS)
- Embryos that are found to be chromosomally normal are considered suitable for transfer to the uterus.
- The embryos that are chromosomally normal are then transferred to the uterus.
It should be noted that PGS is not recommended for everyone and it is best to consult with a specialist to determine whether it is appropriate for you.
Grading of embryos:
Embryos are typically graded based on their appearance and developmental stage, with the highest-grade embryos being considered the most viable for transfer. This includes grading the number of cells, the quality of the cells and the fragmentation.
Grading of embryos is an important step in the PGS process, as it allows doctors to select the embryos that are most likely to result in a successful pregnancy. Additionally, it can also help to reduce the risk of miscarriage and chromosomal disorders such as Down Syndrome.
The grading of embryos is typically done by an embryologist who examines the embryos under a microscope. The embryologist will look at the number of cells in the embryo, the quality of the cells, and the degree of fragmentation (the breaking up of cells) in the embryo.
It is important to note that grading of embryos is a subjective process and different embryologist might have different opinion.
The grading of embryos is done by embryologists and typically involves evaluating several factors, including:
- Cell number: The number of cells in the embryo is evaluated to determine if the embryo is dividing and growing properly.
- Symmetry: The symmetry of the embryo is evaluated to determine if the embryo is developing normally.
- Fragmentation: The degree of fragmentation in the embryo is evaluated, as a high degree of fragmentation can indicate that the embryo is not developing properly.
- Blastomere size: The size of the cells within the embryo is evaluated to determine if the cells are growing at a normal rate.
- Appearance of nuclei: The appearance of the nuclei within the cells of the embryo is evaluated to determine if the embryo is healthy.
- Trophoblast: The trophoblast (the outer layer of cells) is evaluated to determine if it is healthy and properly formed.
Advantages :
Preimplantation Genetic Screening (PGS) is a genetic testing procedure that is used to evaluate the chromosomal makeup of embryos prior to in vitro fertilization (IVF) transfer.
- Increased chance of pregnancy: PGS can help identify healthy embryos that are more likely to result in a successful pregnancy. This can increase the chances of having a baby for couples who have struggled with infertility.
- Reduced risk of miscarriage: PGS can also reduce the risk of miscarriage by identifying embryos that have chromosomal abnormalities, which are known to increase the risk of miscarriage.
- Reduced risk of chromosomal disorders: PGS can detect chromosomal disorders such as Down Syndrome, allowing couples to make informed decisions about which embryos to transfer.
- Better utilization of IVF cycles: PGS can help couples make the most of their IVF cycles by identifying the best embryos to transfer, which can save couples time, money, and emotional stress.
- Improved genetic counseling: PGS can provide couples with genetic counseling and information about their embryos, which can help them make informed decisions about their reproductive options.
- Gender selection: PGS can also be used for gender selection for family balancing or for avoiding passing on a genetic disorder linked to a specific chromosome.
How safe is PGS testing?
Preimplantation Genetic Screening (PGS) is considered a safe procedure overall, but as with any medical procedure, there are some risks involved.
The main risk associated with PGS is the possibility of a false-positive or false-negative result. PGS testing is not 100% accurate and there is a small chance that the test may not detect a chromosomal abnormality or may indicate an abnormality when there is none.
Another risk is that PGS testing may increase the risk of miscarriage. This is because the procedure involves taking a small number of cells from the developing embryo, which can damage the embryo and reduce its chances of survival. However, the risk of miscarriage associated with PGS is considered to be low, and the procedure is generally considered to be safe.
Additionally, there is a small chance of infection or bleeding associated with the procedure.
It is important to have a discussion with your fertility specialist and genetic counselor to understand the potential risks and benefits of PGS testing and weigh them against your individual needs and preferences.
Overall, PGS is considered a safe procedure with many benefits including reducing the risk of chromosomal disorders and miscarriage.
Limitations:
Despite the promising research results in the area of PGS, the technology has both biological and technical limits.
- False positive or false negative results- PGS testing is not 100% accurate and there is a small chance that the test may not detect a chromosomal abnormality or may indicate an abnormality when there is none.
- Risk of damage to the embryo- PGS testing involves taking a small number of cells from the developing embryo, which can damage the embryo and reduce its chances of survival.
- Limited genetic testing- PGS only tests for chromosomal abnormalities and not for other genetic disorders such as cystic fibrosis or Tay-Sachs disease.
- Cost-PGS testing can be expensive and may not be covered by insurance, making it less accessible for some couples.
- Subjectivity- Grading of embryos is a subjective process; different embryologist might have different opinion.
- Embryo selection-PGS testing can help identify embryos that are more likely to result in a successful pregnancy, but it does not guarantee a successful pregnancy or a healthy baby.
- Limited genetic information- PGS can only provide information about the chromosomal makeup of the embryos, and not about the genetic makeup of the entire genome.
Risks:
- PGS testing is not 100% accurate and there is a small risk of getting a false positive or false negative result.
- PGS testing may increase the risk of multiple pregnancies, which can be associated with increased health risks for both the mother and the babies.
- PGS testing may lead to the discarding of embryos that would have been viable, but appear to
- This testing can be emotionally taxing for couples and can lead to feelings of guilt, disappointment, and stress.
Preimplantation Genetic Diagnosis (PGD):
PGD is the testing of embryos for particular genetic abnormalities that have been identified in one or both parents (s). It is commonly known as PGT-M or preimplantation genetic testing for monogenic diseases and is only used in cases when a specific genetic abnormality has been detected.
PGD has been used to test for an expanding range of illnesses since the 1990s, including balanced chromosomal translocations in one or both parents, Huntington disease, hemophilia, sickle cell disease, Tay-Sachs disease, and cystic fibrosis. PGD is frequently performed on fertile couples who want to minimize the possibility of passing on a known genetic disease to their children. Within the professional community, PGD is a widely accepted tool for achieving this purpose.
Differences between PGS and PGD:
The goal of PGT-M or PGD is to detect defective embryos and prevent them from being put back into your uterus, increasing the chances of having a healthy baby. PGT-M can only be performed if the partner is known to be carriers of a genetic disease. A specialized probe will be developed to test for the specific disorder(s) that a couple is suspected of having. PGT-Aon the other hand, will detect and identify previously unknown chromosomal abnormalities. This is preferable for people who have had miscarriages or failed IVF cycles owing to unforeseen circumstances.
References:
- Nussbaum, R.L., McInnes, R.R. and Willard, H.F., 2015. Thompson & Thompson genetics in medicine e-book. Elsevier Health Sciences.
- Gabbe, S.G., Niebyl, J.R., Simpson, J.L., Landon, M.B., Galan, H.L., Jauniaux, E.R., Driscoll, D.A., Berghella, V. and Grobman, W.A., 2016. Obstetrics: normal and problem pregnancies e-book. Elsevier Health Sciences.
- Brezina PR, Ke RW, Kutteh WH. Preimplantation genetic screening: a practical guide. Clin Med Insights Reprod Health. 2013 Feb 27; 7:37-42 Kim MK, Park JK, Jeon Y, Choe SA, Lee HJ, Kim J, Chang EM, Kim JW, Lyu SW, Kim JY, Kwak IP, Lee WS, Yoon TK. Correlation between Morphologic Grading and Euploidy Rates of Blastocysts, and Clinical Outcomes in In Vitro Fertilization Preimplantation Genetic Screening. J Korean Med Sci. 2019 Jan 10;34(4): e27

