Introduction:
- An antibiotic sensitivity test, also known as an antibiotic susceptibility test, is a laboratory test that is used to determine which antibiotics will be effective in treating a particular bacterial infection. The test is performed by culturing a sample of the bacterium on a plate that contains various concentrations of different antibiotics. The plate is then incubated for a period of time to allow the bacteria to grow. After the incubation period, the plate is examined to determine which antibiotics were effective in inhibiting the growth of the bacteria.
- The results of an antibiotic sensitivity test can help a healthcare provider determine the most appropriate antibiotic to prescribe for a particular infection. It is important to use the correct antibiotic to treat an infection, as using an inappropriate antibiotic can lead to the development of antibiotic resistance, which can make future infections more difficult to treat.
- Antibiotic sensitivity tests are typically performed in a laboratory setting by trained professionals. It is important to follow the instructions of a healthcare provider when taking antibiotics, as incorrect usage can lead to the development of antibiotic resistance and other negative consequences.
Purpose:
The results of an antibiotic sensitivity test can help a healthcare provider determine the most appropriate antibiotic to prescribe for a particular infection. It is important to use the correct antibiotic to treat an infection, as using an inappropriate antibiotic can lead to the development of antibiotic resistance, which can make future infections more difficult to treat.
Antibiotic sensitivity testing is an important part of the management of bacterial infections, as it helps healthcare providers to select the most appropriate antibiotic for a particular infection, which can improve patient outcomes and reduce the risk of the development of antibiotic resistance.
Samples:
Samples for an antibiotic sensitivity test can be collected from various sources, including:
Blood: A blood sample may be collected to test for the presence of bacteria in the bloodstream, which can cause sepsis or other serious infections.
Urine: A urine sample may be collected to test for urinary tract infections, which are caused by bacteria that enter the urinary tract and multiply.
Respiratory secretions: A sample of respiratory secretions, such as sputum or bronchial lavage, may be collected to test for respiratory infections, such as pneumonia or bronchitis.
Wound or abscess: A sample of pus or other discharge from a wound or abscess may be collected to test for the presence of bacteria, which can cause an infection.
Tissue: A tissue sample may be collected during a biopsy procedure to test for the presence of bacteria in a specific area of the body.
Procedure:
Antibiotic sensitivity testing is typically performed in a laboratory setting by trained professionals. The procedure is described in general.:
A sample of the bacterium causing the infection is collected and prepared for testing. This may involve processing the sample to isolate the bacteria and grow a pure culture.

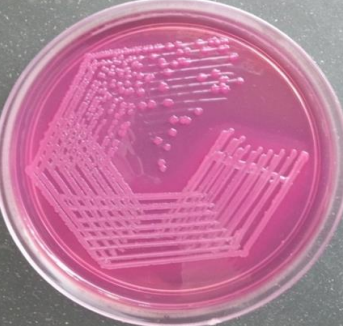
Fig: Procedure of antibiotics sensitivity test
The bacterial culture is placed on a special type of laboratory plate called an antibiotic sensitivity testing plate, which contains different concentrations of various antibiotics.
The plate is incubated for a period of time to allow the bacteria to grow. The length of the incubation period depends on the type of bacteria being tested and the specific testing method being used.
After the incubation period, the plate is examined to determine which antibiotics were effective in inhibiting the growth of the bacteria. This may involve visual inspection of the plate or the use of specialized equipment to measure the growth of the bacteria.
The results of the test are reported to the healthcare provider, who can then use the information to determine the most appropriate antibiotic to prescribe for the infection.
Methods:
There are several methods used to perform antibiotic sensitivity testing, including the following:
Disk diffusion test
This method involves placing a disk impregnated with a specific antibiotic onto a culture plate containing the bacterial strain to be tested. The bacteria grow around the disk and the size of the zone of inhibition (area where bacteria do not grow) is measured.
Dilution test
This method involves creating a series of dilutions of the antibiotic and adding a known number of bacteria to each dilution. The lowest concentration of antibiotic that inhibits the growth of the bacteria is the minimum inhibitory concentration (MIC).
E-test
This method involves using a plastic strip with a gradient of antibiotic concentrations. The strip is placed on a culture plate containing the bacterial strain to be tested, and the MIC is determined by the point at which the bacteria stop growing.
Agar diffusion test
This method is similar to the disk diffusion test, but involves spreading a thin layer of agar onto a culture plate and placing a disk impregnated with the antibiotic onto the agar. The antibiotic diffuses through the agar and the size of the zone of inhibition is measured.
Results:
The results of an antibiotic sensitivity test are reported as either “sensitive,” “intermediate,” or “resistant.”
Sensitive: If the bacteria are sensitive to a particular antibiotic, it means that the antibiotic is effective at inhibiting the growth of the bacteria.
Intermediate: If the bacteria are intermediate to a particular antibiotic, it means that the antibiotic may be effective at inhibiting the growth of the bacteria, but the effectiveness may be reduced compared to bacteria that are sensitive to the antibiotic.
Resistant: If the bacteria are resistant to a particular antibiotic, it means that the antibiotic is not effective at inhibiting the growth of the bacteria.
The results of an antibiotic sensitivity test can help a healthcare provider determine the most appropriate antibiotic to prescribe for a particular infection. It is important to use the correct antibiotic to treat an infection, as using an inappropriate antibiotic can lead to the development of antibiotic resistance, which can make future infections more difficult to treat.
Applications:
Antibiotic sensitivity tests are used in a variety of settings to help healthcare providers determine the most appropriate antibiotic to treat a bacterial infection. Some common applications of antibiotic sensitivity testing include:
Hospital settings: In a hospital setting, antibiotic sensitivity tests may be used to help guide treatment for patients with severe or life-threatening infections, such as sepsis or pneumonia.
Outpatient settings: In an outpatient setting, such as a primary care clinic or urgent care center, antibiotic sensitivity tests may be used to help guide treatment for patients with more minor infections, such as a urinary tract infection or bronchitis.
Long-term care facilities: In long-term care facilities, such as nursing homes, antibiotic sensitivity tests may be used to help guide treatment for patients with chronic infections, such as those with a compromised immune system.
Research settings: In a research setting, antibiotic sensitivity tests may be used to study the effectiveness of different antibiotics against specific types of bacteria, or to investigate the emergence of antibiotic resistance in different populations.
Limitations:
- There are a few limitations to consider when interpreting the results of an antibiotic sensitivity test:
- The test only measures the sensitivity of the bacteria to a specific set of antibiotics. There may be other antibiotics that are effective against the bacteria but were not included in the test.
- The test is performed in a laboratory setting, and the conditions may not fully replicate the conditions in the body. As a result, the test results may not accurately reflect the sensitivity of the bacteria to the antibiotics in the patient.
- The test results may be affected by a number of factors, including the quality of the bacterial sample, the type of testing method used, and the skills and expertise of the laboratory personnel performing the test.
- The results of an antibiotic sensitivity test are only one factor that healthcare providers consider when selecting an antibiotic to treat a bacterial infection. Other factors, such as the overall health of the patient, the severity of the infection, and the potential for side effects, are also taken into account.
Risks:
- There are generally no risks associated with an antibiotic sensitivity test, as it is a laboratory test that is performed on a sample of bacteria and does not involve any direct contact with the patient.
- However, it is important to use the correct antibiotic to treat a bacterial infection, as using an inappropriate antibiotic can lead to the development of antibiotic resistance, which can make future infections more difficult to treat. In addition, using an inappropriate antibiotic can also lead to negative consequences, such as adverse side effects or the failure to effectively treat the infection.
- It is important to follow the instructions of a healthcare provider when taking antibiotics, as incorrect usage can increase the risk of the development of antibiotic resistance and other negative consequences. It is also important to only take antibiotics when they are prescribed by a healthcare provider, as unnecessary use of antibiotics can contribute to the development of antibiotic resistance.
References:
- https://microbiologie-clinique.com/Home.html
- Partridge SR, Kwong SM, Firth N, Jensen SO. Mobile Genetic Elements Associated with Antimicrobial Resistance. Clin Microbiol Rev. 2018 Aug 1;31(4): e00088-17.
- https://medlineplus.gov/
- L. Barth Reller, Melvin Weinstein, James H. Jorgensen, Mary Jane Ferraro, Antimicrobial Susceptibility Testing: A Review of General Principles and Contemporary Practices, Clinical Infectious Diseases, Volume 49, Issue 11, 1 December 2009, Pages 1749–1755